Leuk Res:高 Bax/Bcl-2 比值与 B 细胞慢性淋巴细胞白血病患者的良好预后和更好的生存率相关
2022-01-10 MedSci原创 MedSci原创
较低的 Bax / Bcl-2 比率与较差的预后相关,CLL 患者的 OS 和 PFS 较低就证明了这一点。它还与高肿瘤负荷的标志物和不利的预后标志物有关
在所有白血病中,慢性淋巴细胞白血病(CLL)是全球人群中最普遍的类型。凋亡调节蛋白不仅参与了疾病的发病机制,且在对治疗的反应中也起着重要作用。抗癌药物具有双重作用机制,其中之一是刺激细胞凋亡,因此恶性细胞凋亡异常是耐药的主要机制之一。随着venetoclax等选择性靶向Bcl-2的药物的引入,这在难治性或复发性疾病的CLL患者中升高,识别这类凋亡失调的患者是很重要的。
Bax/Bcl-2 比值的测定可能是识别慢性淋巴细胞白血病 (CLL) 患者的预后和预后以决定治疗时间和类型的良好预测工具,因此,一项前瞻性研究对 100 名新诊断的 CLL 患者进行。

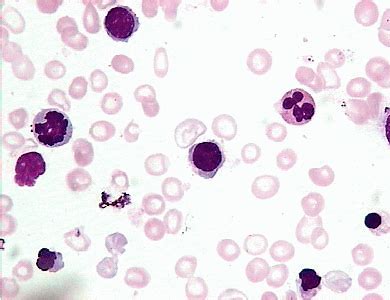
图1:流式细胞术检测2例CLL患者的CD49d、Bax和Bcl-2。A,点图显示淋巴细胞门控的情况。B,点图显示CD49d阳性表达。C,流式细胞术直方图显示高Bcl-2平均荧光强度(MFI)(实心曲线)和低BaxMFI(空心曲线)。D,点图显示淋巴细胞的门控。E,点图显示CD49d阴性表达。F,流式细胞仪直方图显示高BaxMFI(实心曲线)与低Bcl-2MFI(空心曲线)。
通过流式细胞术测量外周血中Bax和Bcl-2的表达。研究了 Bax/Bcl-2 比率与 CLL 实验室标志物、Rai 分期、总生存期 (OS) 和 18 个月时无进展生存期 (PFS) 的关系。评估了 Bax/Bcl-2 在预测生存率方面的敏感性和特异性。
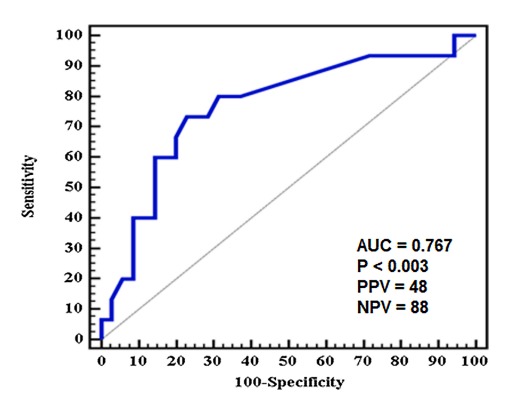
图 2:根据Bax/Bcl-2比值的ROC曲线来预测总生存率。AUC,曲线下的面积。PPV,阳性预测值。ROC,接收机的工作特性。NPV,阴性预测值。P<值为0.05,显著。
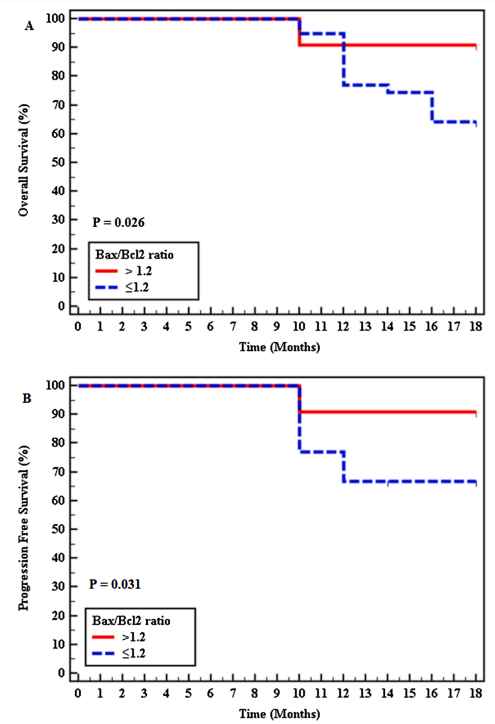
图 3:采用Bax/Bcl-2比值对A,总生存(OS)和B,无进展生存(PFS)的Kaplan-Meier生存分析。P<值为0.05。
通过受试者工作特征 (ROC) 曲线检测,预测生存率的最佳 Bax/Bcl-2 比值为 1.2,敏感性为 80%,特异性为 60.86%。在 78 % 的患者中检测到 ≤1.20 的比率,并且与较差的预后相关。并且在18个月时OS(64.1%对90.9%,p<0.026)和PFS(66.7%对90.9%,p<0.031)显著缩短。在多变量分析中,bax/bcl-2≤1.2是影响总生存率的独立预后因子(p=0.025)。
研究人员得出的结论是,较低的 Bax / Bcl-2 比率与较差的预后相关,CLL 患者的 OS 和 PFS 较低就证明了这一点。它还与高肿瘤负荷的标志物和不利的预后标志物有关。识别具有低 Bax/Bcl-2 比率的患者将使他们成为新型 Bcl-2 抑制性靶向化疗的良好候选者,以避免对传统疗法产生耐药性。
原始出处:
Helaly NA, Esheba NE, Ammo DEA, Elwan NM, Elkholy RA. High Bax/Bcl-2 ratio is associated with good prognosis and better survival in patients with B cell chronic lymphocytic leukemia. Leuk Res. 2021 Aug;107:106604. doi: 10.1016/j.leukres.2021.106604. Epub 2021 Apr 30. PMID: 33965850.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#淋巴细胞白血病#
45
#BCL-2#
36
#BAX#
66
#生存率#
35
#淋巴细胞#
0
血液
56