A&R:具有组织学和临床相关性的青少年局部硬皮病皮肤的转录组学评价
2021-10-08 MedSci原创 MedSci原创
青少年局部硬皮病 (LS)是一种罕见的自身免疫性疾病。这项研究是采用RNA测序(RNA-Seq)比较患青少年LS的儿童皮肤活检组织与健康儿童对照的转录组差异.
青少年局部硬皮病 (LS)是一种罕见的自身免疫性疾病,其发病机制尚未完全清楚。这项研究是采用RNA测序(RNA-Seq)比较患青少年LS的儿童皮肤活检组织与健康儿童对照的转录组差异,发现重要分子靶标。评估差异表达基因(DEGs)与青少年LS儿童的组织病理学和临床特征的相关性,并根据免疫表型将儿童分组为不同的遗传簇。
对28名患青少年LS的儿童和10名儿科健康对照的皮肤组织石蜡包埋切片进行RNA测序。RNA测序使用Illumina HTS TruSeq RNA Access进行文库制备,数据使用STAR对齐,用 DESeq2平台分析。标准化的组织学评分系统用于对皮肤切片的炎症严重程度和胶原沉积水平进行评分。组织学评分由2名对样本状态不知情的病理学家完成。Spearman秩相关系数用于评估青少年LS患者的DEG表达和皮肤组织学发现之间的相关性。
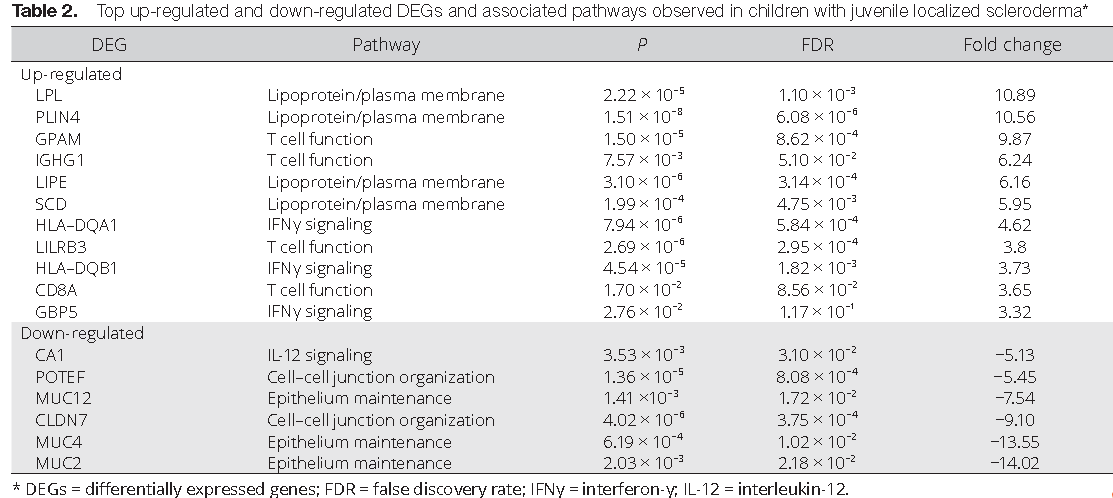
与健康对照相比,研究者在青少年LS儿童中发现了589个显著DEG。分层聚类证明 有3个不同的青少年LS免疫表型簇。基于炎症细胞浸润数量和类别的组织学皮肤炎症评分显著与HLA-DPB1,HLA-DQA2,HLA-DRA和STAT1基因的表达水平相关(rs > 0.5,P < 0.01)。胶原厚度与胶原组织基因的表达水平以及与炎症的严重程度相关的基因有关联,包括主要组织相容性复合体 (MHC) 类别基因I、MHC II和干扰素-γ信号。
结论:
在患有青少年LS的儿童中,确定了3个不同的遗传特征或集群。在一集群,炎症相关通路被上调,对应于更高的皮肤炎症组织学评分。在第二个集群中,纤维化相关通路被上调。在第三组中,皮肤基因表达对应于健康对照中看到的模式。第一簇(以炎症为主)中观察到HLA II基因上调,这一特征在硬斑病患者的外周血液中和系统性硬化症患者的皮肤中也观察到。
出处:
Schutt C, Mirizio E, Salgado C, Reyes-Mugica M, Wang X, Chen W, Grunwaldt L, Schollaert KL, Torok KS. Transcriptomic Evaluation of Juvenile Localized Scleroderma Skin With Histologic and Clinical Correlation. Arthritis Rheumatol. 2021 Oct;73(10):1921-1930. doi: 10.1002/art.41758. Epub 2021 Aug 31. PMID: 33844442.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#相关性#
18
#转录#
29
#组织学#
32
#硬皮病#
33
#局部#
17
#转录组#
37
#评价#
28