Front Oncol:既往接受过抗血管治疗可能影响后线安罗替尼治疗晚期肺癌的PFS,但不影响OS和ORR
2021-12-23 yd2015 MedSci原创
研究表明,既往抗血管生成治疗可能会影响后线接受安罗替尼的PFS,但可能不会影响患者的ORR和OS。
CSCO指南推荐安罗替尼用于晚期肺癌三线或以上治疗。但是既往抗血管治疗(贝伐珠单抗或恩度)是否会影响安罗替尼的疗效尚不明确。因此,来自四川大学华西医院的团队开展了回顾性研究,评估安罗替尼治疗既往抗血管治疗或无抗血管治疗晚期或转移性肺癌(LC)患者的疗效。相关结果发表在Frontiers in Oncology杂志上。
研究回顾性收集使用安罗替尼治疗LC患者的临床资料,将患者分为A组(既往抗血管生成药物失败后使用安罗替尼治疗)和B组(既往未使用抗血管生成药物治疗)。研究使用倾向评分匹配(PSM)平衡两组的混杂因素。分析无进展生存期(PFS)和总生存期(OS)。
共有160例患者纳入分析,其中83例患者既往接受过抗血管生成治疗(贝伐单抗或恩度)(A组),77例患者既往未接受过抗血管生成治疗(B组)。PSM前,两组患者在以下方面不平衡:性别(P=0.020)、年龄(P=0.000)、病理类型(P=0.000)、临床分期(P=0.015)、PD-L1表达水平(P=0.019)、吸烟史(P=0.02)、既往治疗线数(P=0.000)、靶向治疗史(P=0.024)和治疗方案(P=0.014)。
PSM前,A组和B组的ORR和DCR分别为9.6% vs 10.4% (P=0.874)和71.1% vs 80.5% (P=0.165)。PSM后,A组和B组的ORR和DCR分别为13.0% vs 10.9% (P=0.748)和78.3% vs 82.6% (P=0.599)。

PSM前后的疗效评估
对于总体人群,中位OS和PFS分别为14.6个月(95%CI 11.1-18.1)和3.8个月(95%CI 3.1-4.5)。PSM前,A组和B组的中位OS分别为11.8个月和16.1个月(P=0.120),中位PFS分别为3.1个月和4.7个月(P=0.009)。
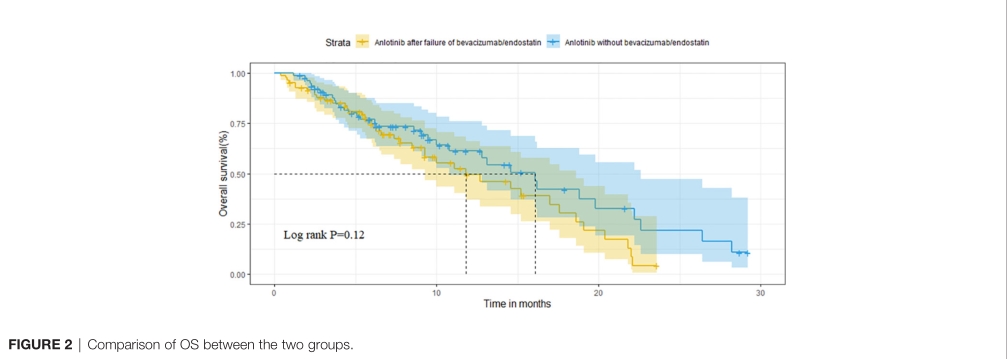
PSM前治疗的OS差异
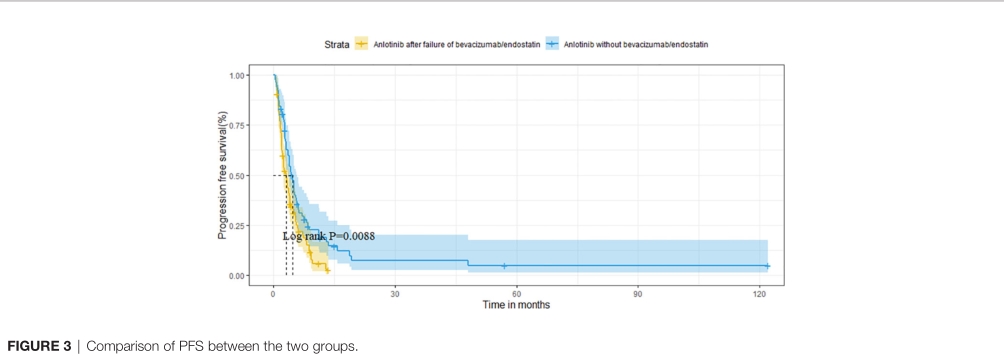
PSM前治疗的PFS差异
PSM后(n=46),两组中位OS分别为14.6个月和16.2个月(P=0.320),中位PFS分别为3.5个月和4.5个月(P=0.040)。
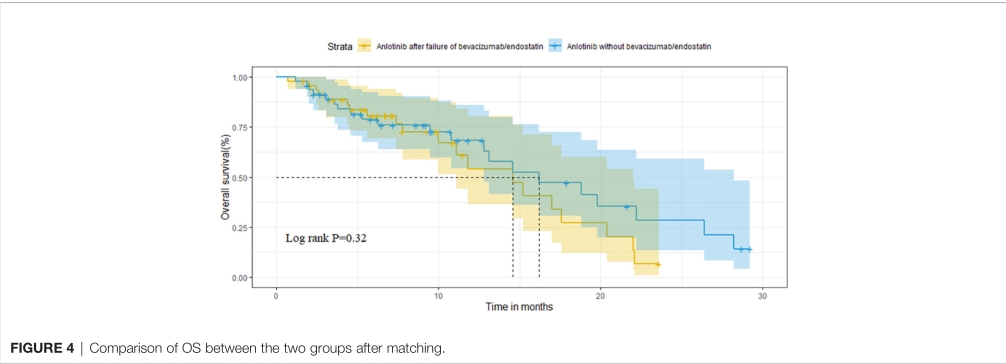
PSM后治疗的OS差异
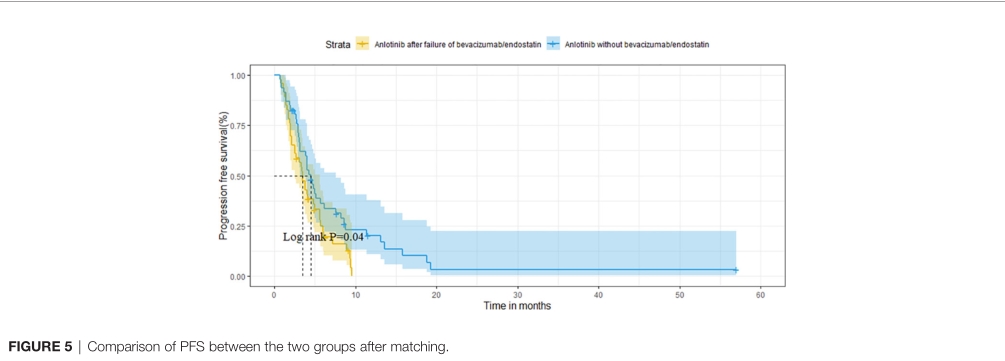
PSM后治疗的PFS差异
为分析既往抗血管生成治疗对安罗替尼治疗的影响,研究进一步分析A组的数据。贝伐珠单抗和恩度治疗的中位PFS分别为3.2和2.1个月(P=0.973)。既往抗血管治疗获得PR、SD和PD患者使用安罗替尼治疗的中位PFS分别为2.7个月,3.1个月和3.8个月(P=0.918)。将既往抗血管治疗的中位PFS分为≤6个月组和>6个月组,安罗替尼治疗的中位PFS分别为2.9和3.3(P=0.592)。
多因素分析,ECOG评分(P=0.002)、脑转移(P=0.006)和肝转移(P=0.006)是PFS的独立预后因素。
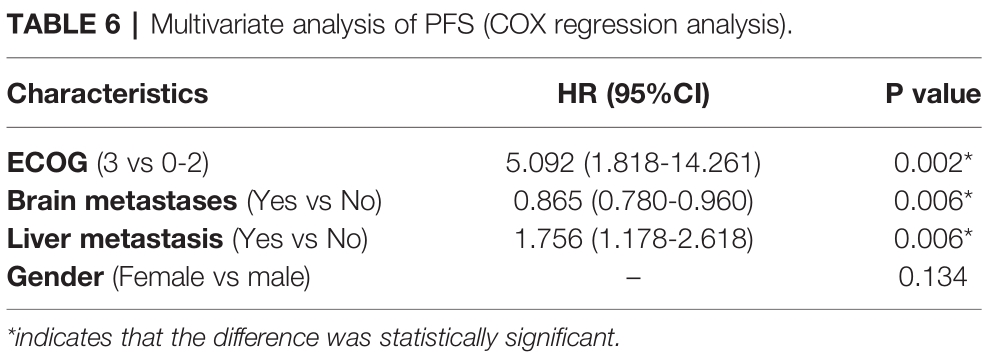
PFS的多因素分析
A组最常见的不良事件是皮肤症状(24.1%),包括皮疹、瘙痒、手足综合征,其次是高血压(8.4%)和疲劳(6.0%)。其他相对罕见的不良事件包括阴道出血(3.6%)、鼻出血(2.4%)和血尿(1.2%)。B组最常见的不良事件是皮肤症状(14.3%)、高血压(10.4%)和厌食症(10.4%),其次是腹泻(7.8%)和疲劳(7.8%)。其他相对少见的不良事件包括:咯血(2.6%)、上消化道出血(1.3%)和中风(1.3%)。
综上,研究表明,既往抗血管生成治疗可能会影响后线接受安罗替尼的PFS,但可能不会影响患者的ORR和OS。
原始出处:
Suo J, Sun Y, Fu Y, Xiu W, Zhang X, Wang Y and Zhu J (2021) A Retrospective Analysis of the Effect of Anlotinib in Patients With Lung Cancer With or Without Previous Antiangiogenic Therapy. Front. Oncol. 11:788837. doi: 10.3389/fonc.2021.788837
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抗血管#
44
#Oncol#
25
#PFS#
44
#ORR#
35
#晚期肺癌#
41