Ann Hematol: 免疫性血小板减少症发展为系统性红斑狼疮的潜在危险因素:中国儿童病例对照研究
2022-05-19 网络 网络
建议对儿科 ITP 患者进行至少 3 年的密切随访,以监测发生 SLE 的风险。高龄和低补体血症是从 ITP 发展为 SLE 的潜在危险因素。
免疫性血小板减少症 (ITP) 患者未来有发展为系统性红斑狼疮 (SLE) 的风险。一研究团队试图通过统计分析探讨中国儿童从 ITP 发展为 SLE 的潜在危险因素。
研究为回顾性病例对照研究。将诊断为 ITP 并在 ITP 诊断后发展为 SLE 的患者定义为病例组。对照组由患有 ITP 但未发展为 SLE 的儿童组成,比例为 1:2。除了单变量分析外,还建立了多变量逻辑回归来评估潜在的危险因素。共纳入150名儿童,其中病例组50名,对照组100名。
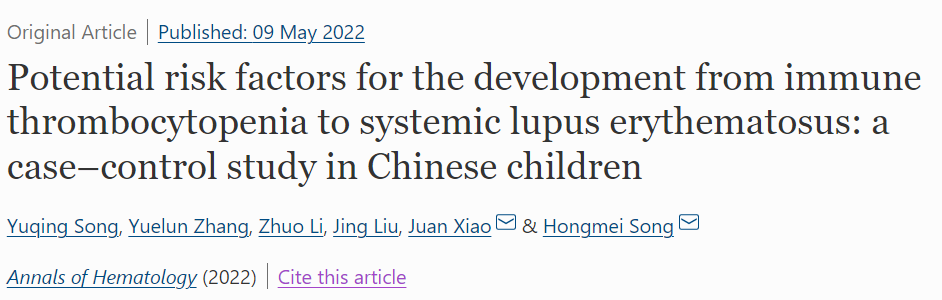
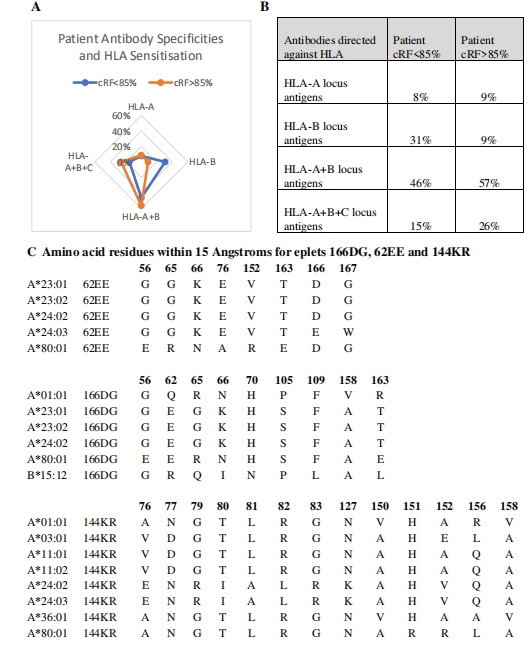
表1:ITP发生SLE组与原发性ITP组的临床表现。缩写:ITP,免疫性血小板减少症;SLE,系统性红斑狼疮;OR,优势比;CI,置信区间;CTD, 结缔组织病
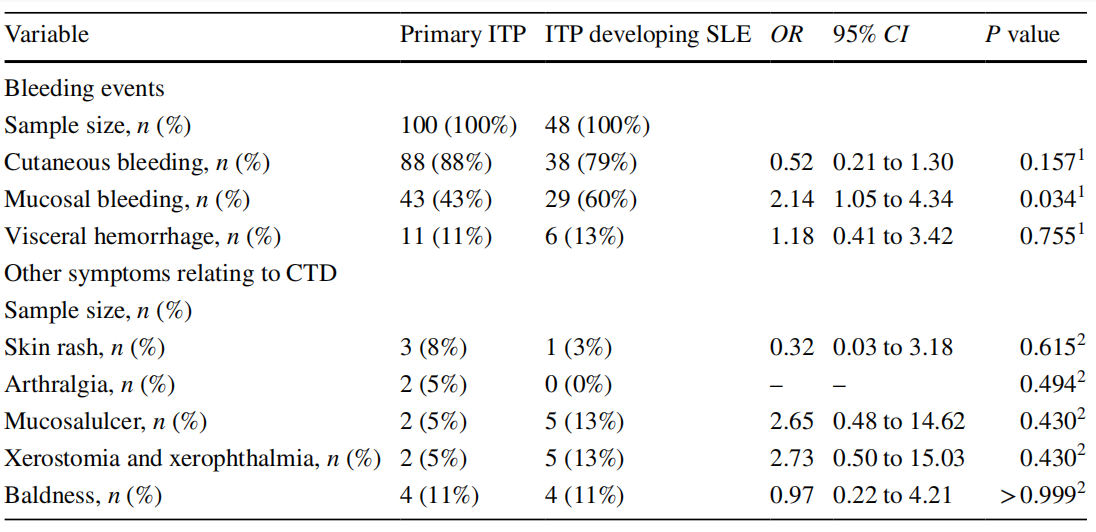
表2:ITP发生SLE组与原发性ITP组之间的血小板和巨核细胞计数

表3:从ITP~SLE等潜在危险因素的多变量分析。缩写:ANA,抗核抗体;C3,补体3;C4,补体4。
从 ITP 到 SLE 的中位发展时间为 34.5 [IQR 12.5, 58.75] 个月。在该研究中,ANA 在单变量分析中发现两组之间存在显著差异,但在多变量分析中没有发现(OR = 4.50,95% CI 0.97 - 21.01)。诊断出的 ITP 与 SLE 呈正相关(OR = 1.07 每 5 年,95% CI 1.01 - 1.15),8 岁时有警报点(敏感性 0.82,特异性 0.60)。较低水平的补体也与 SLE 呈正相关(OR = 8.33,95% CI 1.62 - 42.91)。
综上所述,研究人员首次对50例发展为SLE的ITP患儿和100例未发展为SLE的原发性ITP患儿进行回顾性病例对照研究,探讨发展为SLE的潜在危险因素。从ITP到SLE的中位发展时间为2.9年。
因此,研究建议对儿科 ITP 患者进行至少 3 年的密切随访,对有多种危险因素的患儿进行长达10年的随访,以监测发生 SLE 的风险。随访期间伴有低补体血症的儿童ITP患者未来发生SLE的风险更高。同时,年龄较大的ITP患儿,尤其是8岁以上的患儿,发生SLE的风险明显增加,需要密切随访。ANA阳性可能在一定程度上影响ITP患儿SLE的发展
原始出处:
Song, Y., Zhang, Y., Li, Z. et al. Potential risk factors for the development from immune thrombocytopenia to systemic lupus erythematosus: a case–control study in Chinese children. Ann Hematol (2022). https://doi.org/10.1007/s00277-022-04836-5.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#系统性#
44
#对照#
49
#病例对照#
53
#病例对照研究#
30
#免疫性血小板减少#
39
#血小板减少#
58
#EMA#
36
#狼疮#
28
#红斑#
36