Dig Dis Sci:硫嘌呤单药治疗可有效维持轻中度炎症性肠病患者的临床缓解状态
2022-06-07 xuyihan MedSci原创
炎症性肠病是一类多种病因引起的异常免疫介导的肠道慢性及复发性炎症,有终生复发倾向,溃疡性结肠炎和克罗恩病是其主要疾病类型。
克罗恩病 (CD) 和溃疡性结肠炎 (UC) 是一类复杂的炎症性肠病 (IBD),主要的症状包括瘘管、穿孔、营养不良和肠梗阻。第一种显示对 IBD 有效的药物是 1948 年出现的柳氮磺吡啶,随后在 1960 年代出现了硫嘌呤 6-巯基嘌呤 (6-MP) 和硫唑嘌呤 (AZA) ,这些药物选择性地抑制包括淋巴细胞在内的快速分裂细胞的增殖,而这些细胞在 IBD 的病理生理学中起驱动作用。
最近,在 2015 年进行的一项荟萃分析表明硫唑嘌呤具有维持而不是诱导 IBD 缓解方面的功效。国胃肠病学会 (ACG) 建议将生物治疗作为中重度活动性 IBD 患者的一线治疗,然而,对于轻中度 IBD 患者,尚不清楚这种积极治疗是否必要。对于轻中度 IBD 患者,硫嘌呤单药治疗在维持缓解方面可能仍有作用,这是一种更实惠的替代方案。本研究的目的是评估硫嘌呤单药治疗在维持轻中度 IBD 患者缓解方面的疗效,并确定预测治疗失败的临床因素。
这项回顾性研究纳入了在没有生物治疗的情况下开始使用硫嘌呤的轻度中度 IBD 成人。主要观察结果是疾病治疗失败,以及根据临床、内窥镜和放射学标准定义为疾病进展的情况。在硫嘌呤开始治疗前收集临床变量。单变量和多变量 Cox 比例风险模型用于检查临床变量对治疗反应的独立贡献程度。

在 230名CD患者中64名(72%)没有治疗失败,平均随访时间为3.3年。在多变量模型中,硫嘌呤失败与全身性类固醇给药有关(aHR 2.43,p=0.001),而保护因素包括口服 5-氨基水杨酸(5-ASA)治疗(aHR 0.54,p=0.02)和非瘘管,非狭窄性疾病(aHR 0.57,p=0.047)。在173名 UC 患者中,50 名 (71%) 没有治疗失败,平均随访时间为 3.3 年。在多变量分析中,口服类固醇与硫嘌呤失败有关(aHR 2.71,p=0.001)。只有 13 (4%) 人因不良反应而停用硫嘌呤。
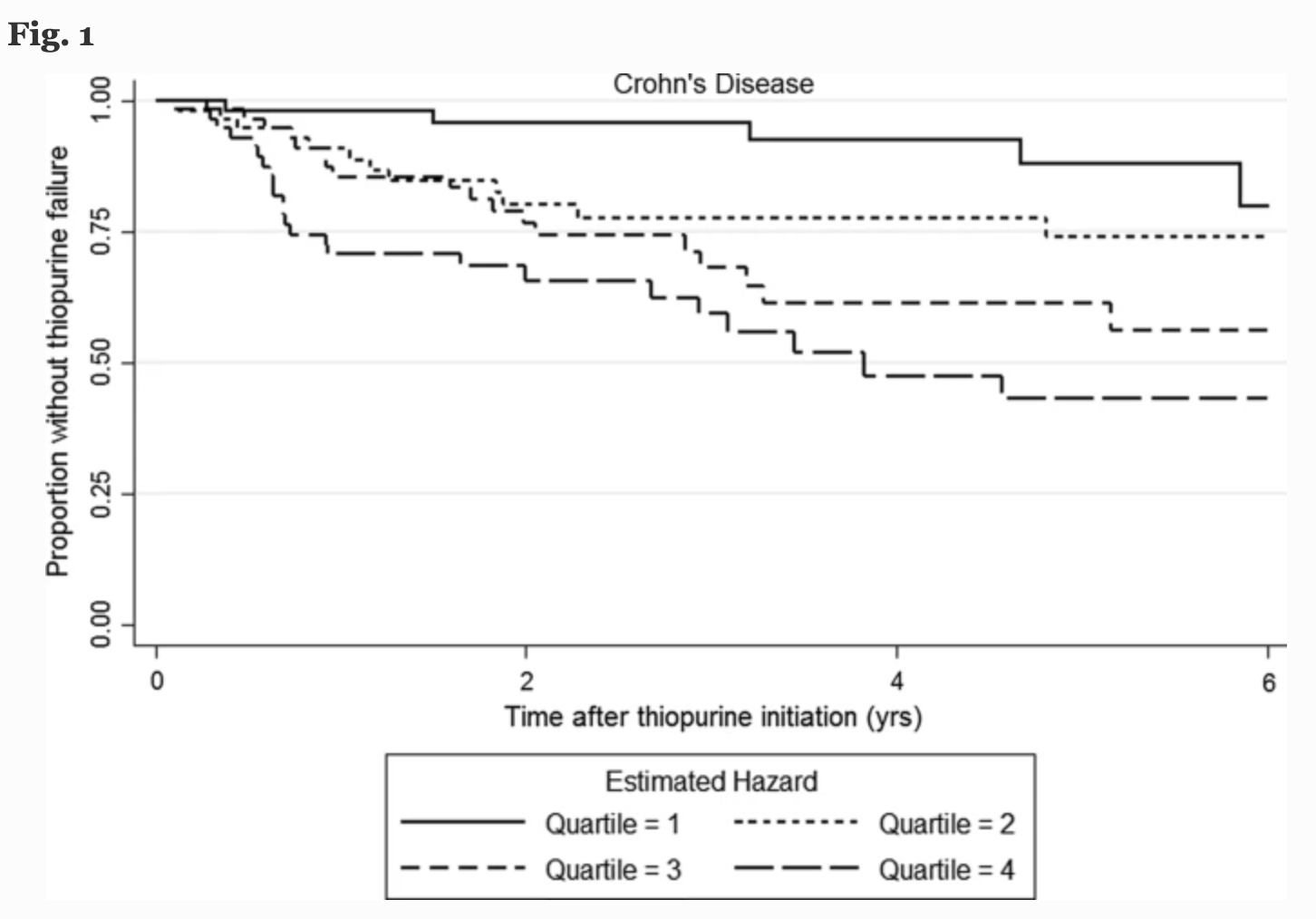
图:患者复发时间图
本项研究证实在轻度中度无并发症 IBD 中,硫嘌呤单药治疗与缓解的临床疾病维持相关,硫嘌呤单药治疗可能代表一种成本更低、方便且有效的生物制剂替代方案。
原始出处:
Grant E. Barber. Et al. Thiopurine Monotherapy Is Effective in Maintenance of Mild-Moderate Inflammatory Bowel Disease. Digestive Diseases and Sciences.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#硫嘌呤#
52
#Dis#
44
#临床缓解#
31
#单药治疗#
44
好好学习
45
已阅读
57
#炎症性#
32
#炎症性肠病患者#
30