J Am Acad Dermatol:天胞疮患者的静脉血栓栓塞风险如何?
2017-05-10 tianxuexin MedSci原创
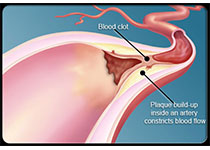
天疱疮是一种自身免疫性粘膜皮肤病,用长期免疫抑制药物治疗。患有天疱疮的患者死亡率增加,有些队列引用静脉血栓栓塞(VTE)作为该群体的重大死因。VTE由肺栓塞(PE)和深静脉血栓形成(DVT)组成,是一个重要的公共卫生问题,主要发生于住院病人,并且是最常见的可预防的住院死因。但是目前对于天疱疮的VTE风险知之甚少。住院治疗患有天疱疮和大疱性类天疱疮共患的患者的VTE风险升高,但天疱疮患者的风险未知。
天疱疮是一种自身免疫性粘膜皮肤病,用长期免疫抑制药物治疗。患有天疱疮的患者死亡率增加,有些队列引用静脉血栓栓塞(VTE)作为该群体的重大死因。VTE由肺栓塞(PE)和深静脉血栓形成(DVT)组成,是一个重要的公共卫生问题,主要发生于住院病人,并且是最常见的可预防的住院死因。但是目前对于天疱疮的VTE风险知之甚少。住院治疗患有天疱疮和大疱性类天疱疮共患的患者的VTE风险升高,但天疱疮患者的风险未知。该项研究的目标是评估一组天疱疮患者的VTE发生率和特征。
研究人员对172例新诊断的天疱疮患者进行了评估VTE发展的回顾性队列研究。
在4年的平均随访时间中,诊断为天疱疮的10例(6%)患者发现了VTE,中位数为4个月。第一年发现VTE风险最高,每100病人每年5次VTE事件或第1年VTE风险5%。 5例患者有深静脉血栓形成,4例有肺栓塞,1例同时存在肺栓塞和深静脉血栓。年龄和性别与VTE风险无关。大多数患者由于天疱疮治疗及其并发症(包括住院治疗,活动固定和感染)或遗传因素而使VTE危险因素增加。
VTE在患有天疱疮的患者中并不罕见,诊断后的第一年更是如此。 必须在所有患者中评估VTE风险,特别是住院时,应在相应病例中开始血栓预防。
原始出处:
Yael Anne Leshem, et al. Venous thromboembolism in patients with pemphigus: A cohort study. Journal of the American Academy of Dermatology. Published online: May 09, 2017.DOI: http://dx.doi.org/10.1016/j.jaad.2017.01.059
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉血栓栓塞风险#
59
#静脉#
28
#静脉血#
32
#ACA#
29