JAHA:二尖瓣脱垂与心脏猝死的关系
2018-11-29 xing.T MedSci原创
由此可见,孤立性MVP和SCD主要影响年轻女性冗余的双叶脱垂,心脏骤停通常由于室性心律失常所致。为了更好地理解MVP和SCD之间的复杂关系,需要通过纵向随访对临床、电生理和心脏成像参数进行标准化报告。
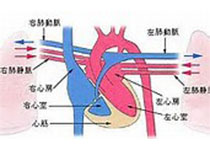
二尖瓣脱垂(MVP)与心源性猝死(SCD)之间的关系仍存在争议。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在该系统评价中,研究人员评估了孤立性MVP和SCD之间的关系,以更好地定义潜在的高风险亚型。此外,研究人员确定生前参数是否可以预测MVP患者的SCD和MVP患者中SCD的发生率。
研究人员对PubMed和Embase数据库中1960年至2018年期间发表的关于MVP和SCD或心脏骤停的所有英文文献进行了检索,还确定了调查室性心律失常或SCD预测因子的文献和报告了MVP患者中SCD结局的队列研究。
研究人员从2180篇引文中共确定了79篇描述了161例发生SCD或心脏骤停的MVP患者的文献。中位年龄为30岁,69%的病例为女性。在47%压力的情况下发生心脏骤停,并且由81%由室颤引起。Holter监测的早产心室复合体(92%)较为常见。大多数病例有双叶受累(70%),冗余(99%)和非严重二尖瓣关闭不全(83%)。从描述MVP患者室性心律失常或SCD预测因子的22篇文献中,小叶冗余是SCD的唯一独立预测因子。MVP患者SCD的发病率估计为每100000人每年217次事件。
由此可见,孤立性MVP和SCD主要影响年轻女性冗余的双叶脱垂,心脏骤停通常由于室性心律失常所致。为了更好地理解MVP和SCD之间的复杂关系,需要通过纵向随访对临床、电生理和心脏成像参数进行标准化报告。
原始出处:
Hui‐Chen Han.et al.Mitral Valve Prolapse and Sudden Cardiac Death: A Systematic Review.JAHA.2018.https://www.ahajournals.org/doi/10.1161/JAHA.118.010584
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#二尖瓣脱垂#
35
#AHA#
38
#二尖瓣#
32
学习了,涨知识了!
82
学习了
67