JAMA Netw Open:中肿麦海强教授团队证实奈达铂为基础的同期放化疗可作为II-IVB期鼻咽癌患者的有效治疗方案
2021-12-27 yd2015 MedSci原创
在这一随机临床试验的二次分析中,长期随访结果证实奈达铂为基础的CCRT可被视为II-IVB型鼻咽癌患者另一种治疗策略。
我们知道,对于II-IVB期鼻咽癌患者,NCCN指南推荐建议以顺铂为基础的同期放化疗。但是顺铂具有较明显毒性,比如肾毒性,胃肠道反应以及神经毒性等。为此,中山大学肿瘤防治中心鼻咽科的麦海强教授团队开展了III期临床研究,比较奈达铂和顺铂为基础同期放化疗治疗II-IVB期鼻咽癌患者的疗效和安全性。初始的分析发现奈达铂非劣效于顺铂。近期,JAMA Network Open杂志更新了其5年随访的生存资料。

这是一项开放标签、非劣效性、多中心随机临床试验的5年随访二次分析,纳入了2012年1月16日至2014年7月16日期间非角化II-IVB期鼻癌患者,中位随访时间为78个月(IQR,3-99个月)。数据分析于2020年11月10日至2021年7月8日进行。主要终点为无进展生存期(PFS)。次要终点为总生存期、远处无转移生存期和局部无复发生存期。
共有402名符合条件的参与者被纳入研究(中位数[IQR]年龄,45[18-65]岁;302[75.1%]男性)。患者被随机分配到以奈达铂为基础或以顺铂为基础的CCRT组(各有201例):196例(97.5%)患者开始以奈达铂为基础的CCRT组,197例(98.0%)患者开始以顺铂为基础的CCRT组。奈达铂组和顺铂组分别只有174例(86.6%)和171例(85.1%)患者进行了血浆EBV-DNA检测,其中奈达铂组血浆EBV-DNA中位浓度为2210 copies/mL (IQR, 0-19150 copies/mL),顺铂组血浆EBV-DNA中位浓度为465 copies/mL (IQR, 0-11300 copies/mL)。
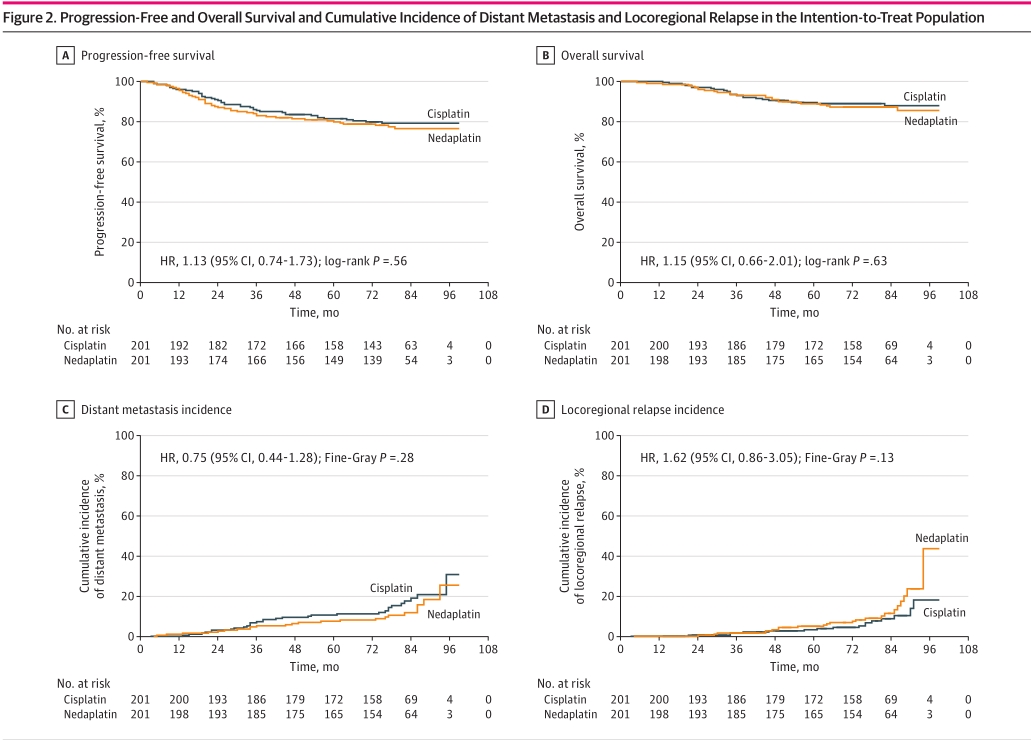
402例患者中,86例(21.4%)发生疾病进展,49例(12.2%)死亡,52例(12.9%)发生远处转移,40例(10.0%)发生局部复发,10例(2.5%)同时发生远处转移和局部复发。ITT人群分析,顺铂组的5年PFS率为81.4% (95%CI,75.9%- 86.9%),奈达铂组为79.8% (95%CI, 74.1%-85.5%) (HR, 1.13; 95%CI, 0.74 1.73;log-rank P = 0.56),差异为1.6%(95% CI, −6.3% to 9.5%; P = .002 for noninferiority)。5年OS率也没有统计学差异(89.4% vs 88.8%; HR, 1.15; 95% CI, 0.66-2.01; log-rank P = 0.63)。两组的远处累计转移率也没有统计学差异(26.9% vs 22.8%;HR,0.75;95%CI,0.44-1.28;Fine-Gray P =0.28)。两组的的局部复发率同样也没有统计学差异(16.7% vs 21.2%; HR, 1.62; 95% CI, 0.86-3.05; Fine-Gray P =0.13)。
预后差异分析
我们对按以下协变量分层的患者进行了OS、PFS、DMFS和LRFS亚组分析:性别(男性或女性)、年龄(45岁或≥45岁),KPS评分(70-80或90-100),疾病分期(II-III或IVA-B)。这些协变量与治疗之间无交互作用(男性:HR,1.14;95%CI,0.71-1.83;女性:HR,1.21; P = 0.49;年龄45岁:HR, 0.92;95%CI,0.48-1.75;年龄≥45岁:HR, 1.36;95%CI,0.77-2.38;P =0.9;KPS 70-80:HR,2.91;95%CI,0.53-15.93; KPS 90-100:HR, 1.07;95%CI,0.69-1.65;P = 0.30; IVA-B期:HR,1.62;95%CI,0.76-3.46;95%CI,0.57-1.59;P =0.61),表明奈达铂为基础的CCRT在特定人群中的非劣性于顺铂-CCRT。
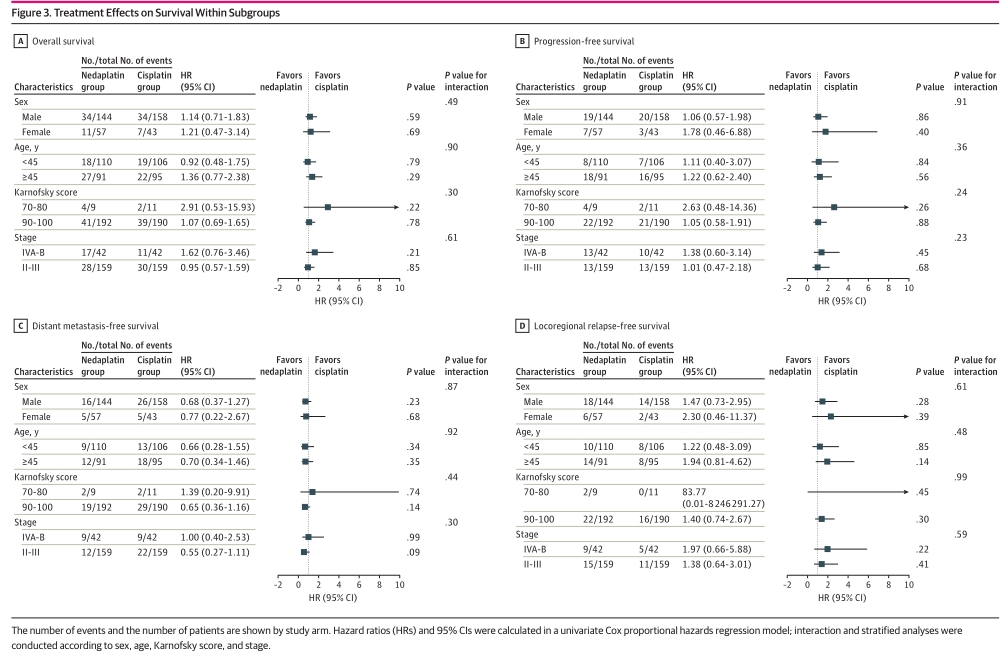
亚组分析
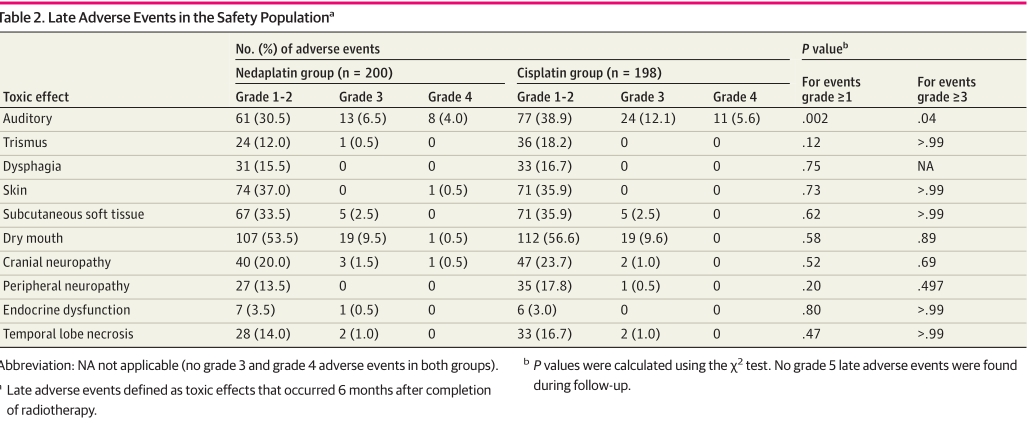
顺铂组患者任何级别或3-4级听觉毒性的发生率显著高于奈达铂组(≥1级:82/200[41.0%] vs 112/198[56.6%], P =0.002; 3-4级:21[10.5%] vs . 35[17.7%],P =0.04)。
不良反应
综上,在这一随机临床试验的二次分析中,长期随访结果证实奈达铂为基础的CCRT可被视为II-IVB型鼻咽癌患者另一种治疗策略。
原始出处:
Tang QN, Liu LT, Qi B, Guo SS, Luo DH, Sun R, Sun XS, Chen DP, Guo L, Mo HY, Wang P, Liu SL, Liang YJ, Li XY, Yang ZC, Chen QY, Mai HQ, Tang LQ. Effect of Concurrent Chemoradiotherapy With Nedaplatin vs Cisplatin on the Long-term Outcomes of Survival and Toxic Effects Among Patients With Stage II to IVB Nasopharyngeal Carcinoma: A 5-Year Follow-up Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open. 2021 Dec 1;4(12):e2138470. doi: 10.1001/jamanetworkopen.2021.38470. PMID: 34928359.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#治疗方案#
45
#铂#
34
#PE#
42
#NET#
44
#同期#
44
学习
59
学习
66
#放化疗#
41
#有效治疗#
48