JNNP:GBA基因变异影响肌萎缩侧索硬化症患者的认知状态
2021-10-02 MedSci原创 MedSci原创
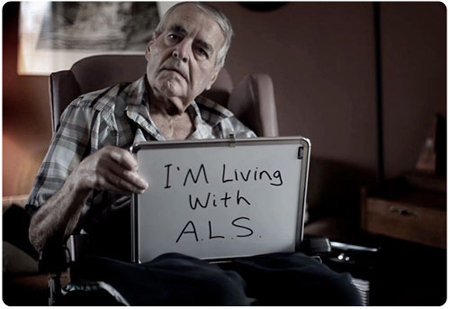
肌萎缩侧索硬化症(ALS)是一种持续进行的上下运动神经元变性疾病。
肌萎缩侧索硬化症(ALS)是一种持续进行的上下运动神经元变性疾病。大约15%的患者表现出与额颞叶痴呆(FTD)相一致的临床特征,35%的患者在其疾病的某个阶段表现出较轻程度的认知和行为损害。据报道,几种基因可导致ALS和FTD。然而,目前尚不清楚为什么一些ALS患者会出现认知障碍,而其他患者(通常在同一个家庭中)却没有受到影响。

GBA基因编码葡萄糖脑苷酶(GCase),这是一种溶酶体酶,可将葡萄糖脑苷转化为葡萄糖和神经酰胺。杂合子GBA突变增加帕金森病(PD)和PD患者认知障碍的风险。 导致孟德尔神经退行性疾病的基因变异可能表现出多效性效应,并影响这些疾病的表型异质性。此外,溶酶体功能障碍最近与路易体痴呆症和FTD谱有关。本文研究GBA变异是否影响ALS患者的认知状态。本文发表在《神经病学,神经外科学和精神病学杂志》上()。
对751例ALS患者进行了GBA变异与认知损害风险的相关性研究,接受了详细的神经心理学评估和全基因组测序筛查。3例患者被归类为认知功能正常的ALS患者(ALS-CN)、ALS-FTD和伴有中度认知缺陷的ALS。
对GBA外显子变异进行突变筛查,并将其与内部对照队列进行比较。以评估是否存在致病性罕见变异。在GBA导致ALS认知能力下降的风险中,如前所述,进行了基于基因的罕见变异关联测试。在分析的下一步中,仅考虑了已知为PD认知能力下降风险因素的变异。首先,使用二项测试评估认知能力下降患者的GBA突变患病率然后,使用线性混合效应模型测试GBA基因型与认知功能之间的相关性,同时包括以下协变量:性别、年龄、发病部位、诊断时的延髓体征、ALS功能评定量表修订率(ALS-FRS-R)下降和C9orf72状态。基于基因的罕见变异关联试验发现伴有中度认知功能障碍的ALS患者中存在丰富的罕见GBA变异(p SKAT-O=0.000005),但在ALS-FTD患者中不存在(p SKAT-O=0.184)。
GBA风险变异携带者的认知表型频率
鉴定了一种已知可导致纯合子携带者Gaucher病的GBA突变、一种可能的致病性变体(p.R209H)和两种已知可增加PD患者痴呆风险的GBA多态性(p.E365K和p.T408M)。与健康对照组相比,队列中GBA变异的频率没有增加。18例ALS患者中有13例(72.2%)携带GBA变异体,表现为FTD或中间认知表型形式的认知障碍。相比之下,47.1%(733名患者中的298名)的ALS患者未携带GBA变异体,观察到认知障碍。通过重复分析排除C9orf72扩增携带者,差异仍然显著(p=0.0486)。为了证实GBA变体对认知表型的影响,使用线性混合效应模型对GBA变体和认知损害之间的关联进行建模。在混合效应模型中,GBA突变状态与认知障碍的临床诊断相关(OR=3.74,95%) CI 1.25至12.72,p=0.023)。当仅考虑ALS-FTD表型或中间表型时,未观察到这种效应。
观察到GBA基因罕见变异的负担与ALS患者的认知障碍相关。与非携带者相比,携带已知致病性GBA变体(p.E365K、p.T408M、p.N409S)的患者发生认知障碍的可能性是非携带者的三倍,与年龄、性别、发病部位、延髓受累、ALS-FRS-R下降率和C9orf72状态无关。认知损害可能随着时间的推移而恶化,并且与更严重的运动障碍相关。诊断时的神经心理学评估可能捕捉到了认知功能障碍轨迹的早期阶段随时间而恶化。
内溶酶体功能障碍参与ALS的发病机制,提示GBA可能在ALS的神经退行性变过程中发挥作用。导致ALS和FTD的几个基因,包括C9orf72、TBK1、OPTN、SQSTM1和VCP,与溶酶体功能和蛋白质降解有关。这一研究领域值得进一步关注,因为针对溶酶体途径的几种治疗药物已被提出用于神经疾病。
总之,本文发现GBA基因的变异与ALS患者认知障碍的风险增加有关。研究结果拓宽了调节ALS患者认知功能障碍易感性的遗传因素的范围,并加强了溶酶体损伤在ALS潜在神经退行性变过程中的作用,强调基因不仅可以改变ALS的风险,还可以调节其表型的不同方面。解决对遗传修饰因子在ALS中所起作用的理解差距对于ALS的诊断、预后和治疗发展至关重要。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#萎缩#
28
#硬化症#
43
#认知状态#
29
#基因变异#
46
#变异#
38
#肌萎缩#
36
#肌萎缩侧索硬化#
51