J Clin Oncol:高风险和极高风险前列腺癌中仅前列腺与全盆腔放射治疗的比较
2021-02-06 AlexYang MedSci原创
最近,有研究人员报告了一项比较高风险前列腺癌中预防性全盆腔结节放疗与单纯前列腺放疗(PORT)的随机试验临床结果。
最近,有研究人员报告了一项比较高风险前列腺癌中预防性全盆腔结节放疗与单纯前列腺放疗(PORT)的随机试验临床结果。
研究为III期、单中心和随机对照试验,共包括了符合条件的患者,这些患者因结节阴性前列腺癌进行了根治性放疗,预估的结节风险≥20%。从2011年11月到2017年8月,共有224名患者随机分配(PORT=114,WPRT=110)。在随访中位数为68个月中,记录了36例生化失败(PORT=25例,WPRT=7例)和24例死亡(PORT=13例,WPRT=11例)。WPRT的5年BFFS为95.0%(95%CI,88.4-97.9),而PORT为81.2%(95%CI,71.6-87.8),未经调整的风险比(HR)为0.23(95%CI,0.10-0.52;P<0.0001)。WPRT同时也显示出更高的5年DFS(89.5% v 77.2%;HR,0.40;95%CI,0.22至0.73;P=0.002),但5年OS没有差异(92.5% v 90.8%;HR,0.92;95%CI,0.41至2.05;P=0.83)。另外,WPRT的远处无转移生存期也较高(95.9% v 89.2%;HR,0.35;95%CI,0.15至0.82;P=0.01)。在不同预后亚组中,BFFS和DFS的获益得以维持。
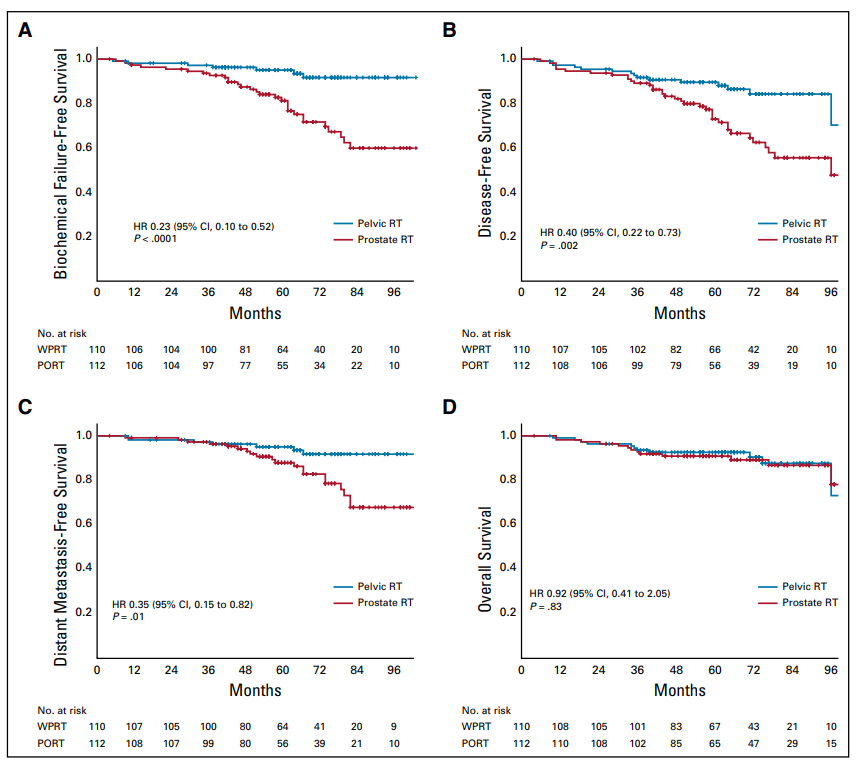
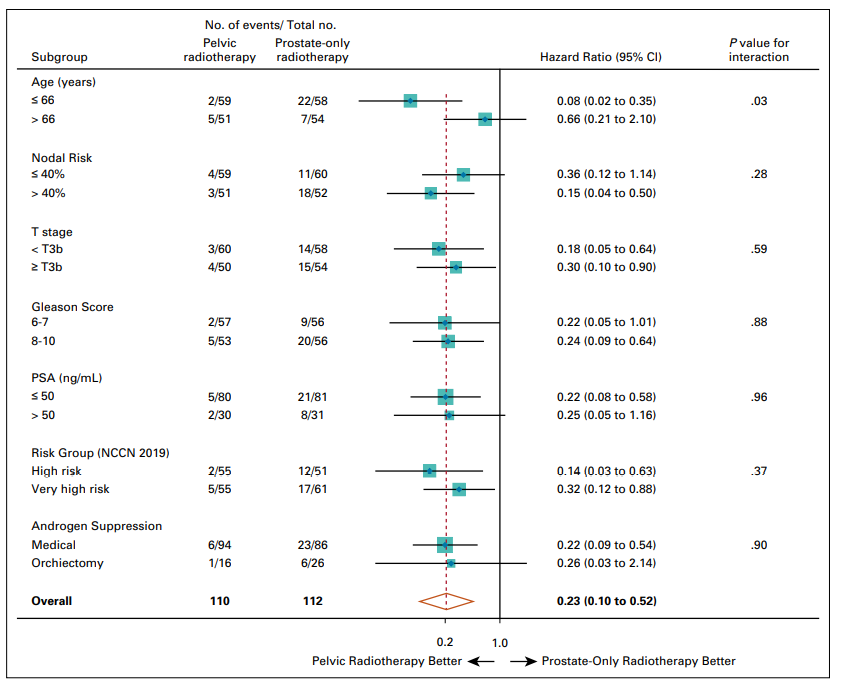
最后,研究人员指出,与PORT相比,高风险和局部晚期前列腺癌的预防性盆腔照射可改善BFFS和DFS,但OS没有差异。
原始出处:
Vedang Murthy , Priyamvada Maitre , Sadhana Kannan et al. Prostate-Only Versus Whole-Pelvic Radiation Therapy in High-Risk and Very High-Risk Prostate Cancer (POP-RT): Outcomes From Phase III Randomized Controlled Trial. J Clin Oncol. Jan 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
37
#高风险#
35
谢谢梅斯分享这么多精彩信息
0
前列腺癌相关研究,学习了,谢谢梅斯
0