气管憩室患者双腔支气管导管定位困难一例
2020-05-07 殷悦 仓静 临床麻醉学杂志
患者,男,53岁,172 cm,55kg,因“咳嗽咳痰伴咯血半年余”入院。既往有肺气肿、支气管扩张病史。6年前因车祸导致右肺挫伤、多发肋骨骨折,行手术治疗(具体术式不详),有气
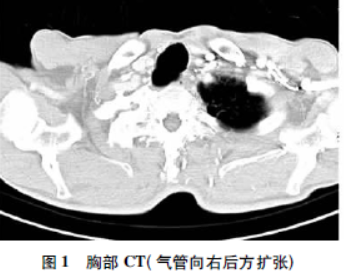
患者,男,53岁,172 cm,55kg,因“咳嗽咳痰伴咯血半年余”入院。既往有肺气肿、支气管扩张病史。6年前因车祸导致右肺挫伤、多发肋骨骨折,行手术治疗(具体术式不详),有气管切开史及输血史。否认吸烟史,少量饮酒。查体:双肺呼吸音粗,心律齐,腹部平软,双下肢无水肿。胸部CT:两肺气肿,两肺支气管扩张伴感染,右肺上叶为著(图1)。
肺功能:轻度混合型通气功能障碍,一氧化氮弥散中度下降,FEV12.23L,FEV1/FVC98.27%。支气管镜检查:气管上段右侧壁局部呈牵拉性扩张,部分软骨环消失,管腔通畅,隆突锐利(图2)。

诊断为右上肺毁损肺,拟行右上肺叶切除术。术前血常规:RBC4.69×1012/L,Hb135g/L,WBC6.24×109/L,中性粒细胞63.4%,PLT199×109/L。肝肾功能:ALB39g/L,ALT14U/L,AST19U/L,Scr75mmol/L,BUN7.1mmol/L。凝血功能:PT12.6s,APTT35.2s,INR1.09。
专科检查:牙齿完整,颈部活动度好,张口度>3 cm,颏甲间距>6.5 cm,MallampattiI级。患者入室后行硬膜外穿刺置管及右颈内静脉穿刺置管。连接II、V五导联心电图,监测无创动脉血压及SpO2。HR72次/分,BP110/68mmHg,SpO2 99%。麻醉诱导给予丙泊酚TCI4.0μg/ml,瑞芬太尼TCI0.2μg·kg-1·min-1,舒芬太尼20μg,罗库溴铵40mg。普通喉镜暴露下Cormack-Lehane评分I级,置入39Fr双腔管(管体外径13mm),通过声门下1~2 cm时阻力较大,考虑患者既往气管切开史,声门下狭窄可能,随即更换37Fr双腔管(管体外径12.3mm),插管过程顺利,导管支气管端顺利进入左主支气管。纤支镜定位后依次给气管套囊及支气管套囊注气,气管套囊注气(>10ml)后见双腔管明显移位、导管支气管端滑出左主支气管。
重新调整导管位置,再次定位后先予支气管套囊注气(3ml),双腔管无移位,气管套囊注气(>10ml)后双腔管再次滑出左主支气管。反复尝试(增加导管深度、颈部屈曲)仍定位失败。最终予支气管套囊注气3ml、气管套囊注气5ml,再次纤支镜定位,发现导管放置到位,未见导管再次滑出。固定双腔管(距门齿30 cm),连接呼吸机机械通气,开始手术。
麻醉诱导及气管插管术后行血气分析:pH7.28,PaO2150mmHg,PaCO252mmHg,BE-2.8mmol/L,乳酸0.5mmol/L,血糖6.9mmol/L。术中单肺通气时FiO270%~80%,维持PETCO245~50mmHg,根据需要间断硬膜外注射0.15%布比卡因,静脉注射舒芬太尼及顺式阿曲库铵。最终行右上肺叶切除术+胸膜烙断术,手术时间6h,术中出血约2000ml,输晶体2000ml,胶体1000ml,血浆400ml,少浆血800ml,术毕尿量400ml。术毕待患者符合拔管指征后拔除双腔支气管导管并转至外科监护室。
入监护室时HR68次/分,BP96/51mmHg,SpO2100%。血气分析:pH7.30,PaO2197mmHg,PaCO247mmHg,Hb83g/L,BE-3.2mmol/L,乳酸1.2mmol/L。术后第2天转入普通病房,2周后出院。为进一步明确双腔管定位困难原因,术后第3天行气管三维重建CT,结果提示气管憩室,憩室位于隆突上5.6 cm左右,长度(与气管平行)约3.5 cm,最大横径约3.2 cm。
讨论
气管憩室是一种累及气管和主支气管、突出于气管和支气管腔外的囊性病变。此种疾病较罕见,发病率在成人和儿童分别约为1%和0.3%。气管憩室可分为先天性和获得性两种类型。先天性憩室一般较小,与气管连接处狭窄,常位于声门下4~5 cm或隆突上,憩室壁包含平滑肌、软骨、呼吸道上皮组织等类似正常气管壁的结构。获得性憩室一般偏大,多以广口与气道相连,常位于气管右后侧壁,憩室壁大多由呼吸道上皮组织构成。气管憩室可无明显临床表现,仅由CT、支气管镜或活检偶然发现,大的憩室可以作为脓性分泌物的“储存库”,致使反复呼吸道感染、咳嗽、咳痰、呼吸困难、咯血、声嘶、颈部脓肿、吞咽困难等。
无症状的气管憩室无需积极治疗,反复感染的老年患者可给予对症支持治疗,外科手术则更适用于儿童。本例患者有肺气肿、支气管扩张及肺部外伤病史,气道内慢性压力增高引起获得性憩室可能性大。Goo等指出,有长期咳嗽咳痰病史的慢性阻塞性肺病(COPD)患者要警惕气管憩室的可能。气管憩室的临床表现、肺功能测定、影像学表现与COPD类似,两种疾病有一定的相关性。气管憩室对麻醉的影响主要有插管困难、通气困难、正压通气相关并发症等。
Salhotra等曾报道一例困难插管11岁男性患儿,患有Lesch-Nyhan综合征,在全身麻醉气管插管时6.0#气管导管声门下1 cm“难以通过”,术后CT显示声门下9mm气管憩室,且憩室远端3.5 cm气管异常狭窄(<0.5 cm),由此推断困难插管是气管导管误入憩室盲端所致。除此之外,气管导管误入憩室还会引起通气困难。
Davies报道的一例预料外的困难插管,也是继发于声门下的气管憩室加上气管极度屈曲(几乎成90°),最终气管插管失败,以喉罩通气完成手术。因此,确诊气管憩室或可疑气管憩室行择期手术的患者术前应行气管三维重建CT明确憩室的大小、位置(与声门及隆突的关系)、有无气管异常狭窄。气管憩室壁较正常气管壁薄弱,尤其是获得性憩室壁大多由呼吸道上皮组织构成,正压通气下有憩室穿孔的风险。
有文献报道一名90岁男性患者全麻插管后出现皮下及纵膈气肿,支气管镜检查吸气相声门下4 cm见0.5 cm×2.5 cm大小气管憩室,呼气相憩室塌陷。纵膈气肿疑似正压通气时憩室穿孔引起。Allaert等报道一例全麻插管后双侧颈部及上胸部皮下气肿,术后发现隆突上3 cm气管憩室。因此,确诊气管憩室的患者为避免气道相关问题首选区域麻醉,其次全身麻醉喉罩通气(尽可能保留自主呼吸),最后是全身麻醉气管插管。必需气管插管的患者,选择合适型号的气管导管,事先预估憩室和导管尖端及套囊的位置关系,或者插管后应用支气管镜观察憩室的开口是否封闭,尽量避免憩室位于导管尖端远端,以免术中通气压力过高引起憩室穿孔。如有必要,选择双腔支气管导管代替单腔管封闭憩室开口。
有报道首次全麻插管后引起憩室穿孔,二次全身麻醉时麻醉医生选择双腔支气管导管顺利完成手术。本例患者憩室位于隆突上5.6 cm左右,气管上段部分软骨环消失,气道支撑力及弹性减弱,而双腔支气管导管气管套囊位置邻近憩室,导致气管套囊大量注气后导管支气管端极易滑出左主支气管。考虑该患者气管憩室的位置,若日后需要气管插管,正压通气有憩室穿孔的风险,气道管理上需高度注意。
综上所述,气管憩室患者可无明显临床表现,仅由CT三维重建、支气管镜或活检偶然发现,在无辅助检查的前提下难以确诊。加上憩室大多存在于主气道,一些位置较高接近声门,胸部CT易漏诊,这便需要麻醉医生增强对此疾病的认识并锻炼术前读片的能力,尤其对于有气道损伤或气管切开史等高危因素的患者,能及时识别气管憩室及其对气道建立的影响,给出正确的处理。
原始出处:
殷悦,仓静.气管憩室患者双腔支气管导管定位困难一例[J].临床麻醉学杂志,2019,35(05):519-520.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#支气管#
19
#气管憩室#
36
#气管导管#
30
#憩室#
26