Lancet Oncol:新辅助放化疗加用Galunisertib可提高局部晚期直肠癌的完全缓解率
2022-08-10 MedSci原创 MedSci原创
新辅助放化疗方案加用Galunisertib可将局部晚期直肠癌患者的完全缓解率提高到 32%
TGF-β是一种免疫抑制细胞因子,在结直肠癌中上调。 TGF-β阻断可改善结直肠腺癌临床前模型对放化疗的反应。该研究旨在验证以下假设:在新辅助放化疗中加用 TGF-β I 型受体激酶抑制剂 Galunisertib 可提高局部晚期直肠癌患者的病理完全缓解率。
这是一项由调查者发起的、单臂的2期研究,招募了年满18岁既往未治疗过的、局部晚期的IIA-IIIC或IV期直肠腺癌患者,在基于氟尿嘧啶的放化疗前和过程中,予以两个14天疗程的口服 Galunisertib(150 mg,2次/日)。5-9周后,评估患者的的治疗反应。完全缓解的患者可以选择非手术治疗,即改良的 FOLFOX6 或 CAPEOX 治疗。未完全缓解的患者接受手术切除。主要终点是完全缓解率。
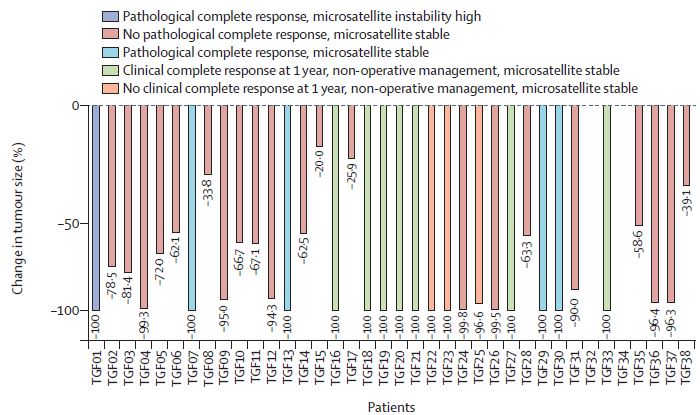
受试患者的肿瘤反应
2016年10月19日-2020年8月31日。共招募了38位患者。35位完成放化疗的患者中有25位(71%)进行了全直肠系膜切除术,其中5位(20%)获得了病理完全缓解。10 位 (29%) 患者接受了非手术治疗,其中 3 位 (30%) 最终选择了全直肠系膜切除术。这三位患者中有两位(67%)获得了病理完全缓解。在非手术治疗组的其余 7 位患者中,5 位 (71%) 在最后一次改良 FOLFOX6 用药后 1 年获得临床完全缓解。总体上,38位患者中有12位(32%)获得了完全缓解。
治疗期间常见的 3 级不良事件包括腹泻(16%),以及血液学毒性(18%)。两位 (5%) 患者出现 4 级不良事件,一位与放化疗引起的腹泻和脱水有关。无治疗相关死亡病例。
综上,在局部晚期直肠癌患者的新辅助放化疗方案加用 Galunisertib 可将完全缓解率提高到 32%,且耐受性良好,值得在随机试验中进一步验证。
原始出处:
Tomoko Yamazaki, et al. Galunisertib plus neoadjuvant chemoradiotherapy in patients with locally advanced rectal cancer: a single-arm, phase 2 trial. Lancet Oncol. August 08, 2022. https://doi.org/10.1016/S1470-2045(22)00446-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#辅助放化疗#
44
#新辅助#
36
#完全缓解#
41
#Lancet#
32
#局部晚期#
51
#Oncol#
33
#局部晚期直肠癌#
40
#放化疗#
37
#局部#
44
#新辅助放化疗#
40