赛诺菲:Dupixent(dupilumab)治疗严重慢性鼻窦炎、鼻息肉的两项III期临床试验取得了积极成果
2019-02-26 不详 网络
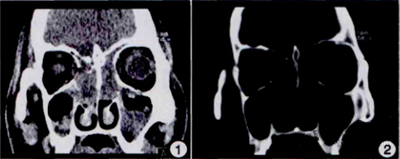
两项III期试验(SINUS-24和SINUS-52)对患有复发性慢性鼻窦炎和鼻息肉(CRSwNP)的患者进行了详细的研究,这些患者先前接受了手术和/或全身性皮质类固醇治疗。Dupixent(dupilumab)在加入到标准皮质类固醇鼻腔喷雾剂时可改善鼻息肉大小、鼻充血严重程度、慢性鼻窦疾病、嗅觉和咳嗽。
两项III期试验(SINUS-24和SINUS-52)对患有复发性慢性鼻窦炎和鼻息肉(CRSwNP)的患者进行了详细的研究,这些患者先前接受了手术和/或全身性皮质类固醇治疗。Dupixent(dupilumab)在加入到标准皮质类固醇鼻腔喷雾剂时可改善鼻息肉大小、鼻充血严重程度、慢性鼻窦疾病、嗅觉和咳嗽。在严重的患者中,Dupixent减少了全身使用皮质类固醇的需要以及鼻/鼻窦手术的需要。这些数据是在2019年美国过敏、哮喘和免疫学会(AAAAI)年会上提出的。
患有CRSwNP和哮喘的共病患者通常更难以治疗,但SINUS-24和SINUS-52的积极结果是令人鼓舞的。Dupixent是一种人单克隆抗体,专门用于抑制白细胞介素-4和白细胞介素-13(IL-4和IL-13)的信号传导。这些研究的结果,以及先前对特应性皮炎和哮喘的研究表明,IL-4和IL-13是在2型炎症中起重要作用的两种关键蛋白质,它们似乎是CRSwNP以及几种过敏性疾病的基础。
原始出处:
http://www.firstwordpharma.com/node/1626711#axzz5gd5Pbuy9
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#II期临床试验#
24
#Dupixen#
42
#mAb#
26
#I期临床#
48
#I期临床试验#
21
#III#
40
#Dupilumab#
30
#慢性鼻窦炎#
29
#Dupixent#
43
#II期临床#
20