JACC子刊:葛均波院士团队发现下腔静脉触发点,也可引发房颤!
2022-08-26 中国循环杂志 中国循环杂志 发表于威斯康星
下腔静脉是阵发性房颤的一个罕见但潜在的触发位点,可通过局部射频消融来识别和安全消除。
在房颤射频消融过程中,识别肺静脉以外的房颤触发位点有着非常重要的意义。
近期,复旦大学附属中山医院葛均波院士、上海交通大学附属第一人民医院刘少稳教授等发表在JACC临床电生理子刊上的一项研究表明,下腔静脉是阵发性房颤的一个罕见但潜在的触发位点,可通过局部射频消融来识别和安全消除。
该研究显示,隔离肺静脉后,来源于下腔静脉的异位搏动,在心电图所有导联表现为窄P'波间期和负向P'波。
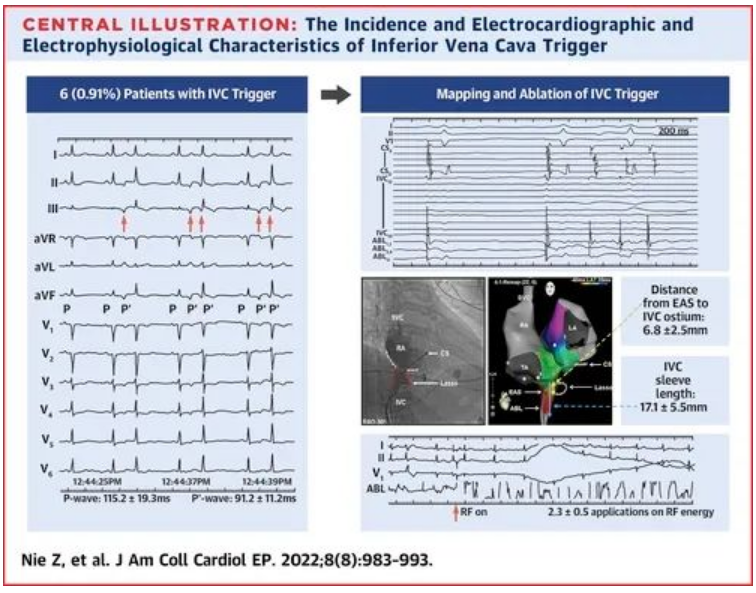
该研究一共纳入661例接受初始阵发性房颤消融的患者,隔离肺静脉后,通过多极标测和血管造影,发现6例(0.91%)患者出现了来自于下腔静脉的房颤。
从最早的激动部位到下腔静脉口的平均距离为6.8 mm。而且,下腔静脉内的致心律失常位点均位于下腔静脉的心尖半球。共用了2.3次射频能量来消除下腔静脉触发灶。
在心电图上,异位P波(P'波)的平均间期为91.2 ms,这比正常的窦性P波窄得多(115.5 ms)。而且,胸前导联的所有P'波均呈负向。
平均随访25.5个月后,这6例患者在未用抗心律失常药物的前提下,均未出现心律失常。
来源:Inferior Vena Cava as a Trigger for Paroxysmal Atrial Fibrillation: Incidence, Characteristics, and Implications. JACC Clin Electrophysiol. 2022, 8(8): 983-993.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
90
#JACC#
69
#下腔静脉#
60
#葛均波#总有新的发现#房颤#
0
#ACC#
60
#葛均波院士#
44