吕树铮:>50%的不明胸痛症状源于颈胸椎疾病
2016-09-03 吕树铮 中华心血管病杂志
临床中,常会遇到所谓“不典型胸痛”的患者。心血管疾病、呼吸系统疾病、纵膈疾病、胸廓疾病、腹腔脏器疾病等均可引起胸痛,而安贞医院吕树铮教授提醒临床医生,还有颈椎病。 颈椎病,又称颈椎综合征,是颈椎骨关节炎、增生性颈椎炎、颈神经根综合征、颈椎间盘脱出症的总称。这类疾病在人群中较为常见,全国有7%~10%的人有颈椎病,而且随年龄增长发病率升高,到60岁左右有一半人,70岁左右则近100%。
临床中,常会遇到所谓“不典型胸痛”的患者。心血管疾病、呼吸系统疾病、纵膈疾病、胸廓疾病、腹腔脏器疾病等均可引起胸痛,而安贞医院吕树铮教授提醒临床医生,还有颈椎病。
颈椎病,又称颈椎综合征,是颈椎骨关节炎、增生性颈椎炎、颈神经根综合征、颈椎间盘脱出症的总称。这类疾病在人群中较为常见,全国有7%~10%的人有颈椎病,而且随年龄增长发病率升高,到60岁左右有一半人,70岁左右则近100%。
而由颈胸椎疾病引起的胸痛称为颈胸综合征。据统计,50%以上的不明原因胸痛和胸闷等症状源于颈胸椎疾患。
吕树铮介绍说,颈椎病增生的骨质压迫或刺激颈神经根、脊髓或交感神经均可引起患者胸痛和胸闷等不适症状。
颈椎病引起急性胸痛有几个特点:
(1)放射至上肢的疼痛部位为臂、拇指和食指的外侧和背侧,而非无名指和食指,这与心绞痛不同;
(2)由颈部运动、体位变动或特定姿势下(如低头、上肢用力或举起动作等)引发,多为突然性阵痛,可自动消失,也可能会隐隐作痛几个小时;
(3)硝酸甘油等药物多无效;
(4)多无心电图及影像学的心肌缺血性改变。
不过,在考虑颈椎病时,也还需进行相应的冠心病筛查。此外还要做好其他相应症状的鉴别诊断,如眩晕者,需注意排除耳源性眩晕、眼源性眩晕、脑源新眩晕等;颈肩上肢痛需与肩周炎、风湿性关节炎和胸廓出口综合征等相鉴别。
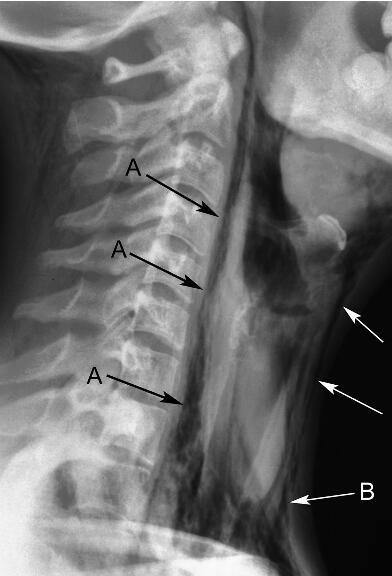
对于心内科介入医生,吕树铮提醒,在冠状动脉造影过程中,除了要观察患者冠状动脉走行及管腔通畅情况外,还需同时注意患者颈椎及胸椎情况,观察有无过度骨质增生、骨赘和骨桥形成等现象。尤其在冠状动脉未见明显狭窄时,不宜轻易下“心脏X综合征”诊断,而遗漏颈椎病的病因诊断。
对于冠状动脉存在严重狭窄而行支架术的患者,亦不应忽视合并颈椎病的问题,应向患者解释清楚,冠心病的治疗方案无法缓解颈椎病所引起的不适,患者仍可能存在胸痛,以取得患者的理解和合作。
来源:吕树铮. 注意颈椎病引起的胸痛. 中华心血管病杂志, 2016,44(07): 563-564.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












让我耳目一新
76
#颈胸椎#
31
颈椎病增生的骨质压迫或刺激颈神经根、脊髓或交感神经均可引起患者胸痛和胸闷等不适症状。好文,值得推荐。
77
很好,不错,以后会多学习
72
很好,不错,以后会多学习
73
学习了啊
74
#胸椎#
33
值得学习
0
值得学习
32
值得学习
25