Blood:转录因子ETS1调控NK细胞发育和终末分化
2020-05-04 QQY MedSci原创
人ETS1缺乏会抑制几种NK细胞相关关键转录因子的表达和NK细胞的分化。 ETS1对于肿瘤细胞诱导性NK细胞毒性和IFN-γ的产生必不可少。
人ETS1缺乏会抑制几种NK细胞相关关键转录因子的表达和NK细胞的分化。
ETS1对于肿瘤细胞诱导性NK细胞毒性和IFN-γ的产生必不可少。
摘要:
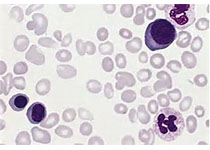
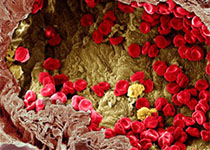
自然杀伤细胞(NK)在肿瘤细胞和病原体的免疫防御中发挥重要作用,并通过细胞因子的分泌调节其他免疫细胞。虽然小鼠NK细胞的生物学已经被广泛研究,但有关转录通路调控人类NK细胞发育和成熟的知识却很有限。
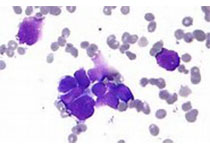
通过产生ETS1缺陷的人类胚胎干细胞(hESC)和在脐血(CB)造血祖细胞(HPCs)中表达显性阴性ETS1 p27亚型,研究人员发现转录因子ETS1是人NK细胞分化的关键因子。
RNA测序结合染色质免疫沉淀(ChIP-seq)的全基因组转录组分析显示,人类ETS1可直接诱导控制NK细胞分化的关键转录因子E4BP4、TXNIP、TBET、GATA3、HOBIT和BLIMP1的表达。
此外,ETS1还调控凋亡和NK细胞活化相关基因的表达。
本研究揭示了ETS1作为人类NK细胞发育和终末分化的重要调控因子的分子机制。
原始出处:
Sylvie Taveirne,et al. The transcription factor ETS1 is an important regulator of human NK cell development and terminal differentiation. Blood. April 29, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#转录#
26
#ETS1#
33
#发育#
28
#转录因子#
33