椎-基底动脉扩张延长症致面肌痉挛的手术治疗
2019-06-13 丁胜超 贺峰 贾继明 中国临床神经外科杂志
2014年7月至2017年7月收治HFS110例,其中7例为VBD致HFS,男2例,女5例;年龄37~63岁,平均(50±7)岁;左侧5例,右侧2例;症状持续时间为6个月至12年,平均(3.7±1.9)年。
1. 资料与方法
1.1 研究对象
2014年7月至2017年7月收治HFS110例,其中7例为VBD致HFS,男2例,女5例;年龄37~63岁,平均(50±7)岁;左侧5例,右侧2例;症状持续时间为6个月至12年,平均(3.7±1.9)年。
1.2 影像学检查
术前采用西门子3.0 T磁共振机进行头部MRI检查,联合应用三维时间飞跃法血管成像序列(three dimensional time of flight,3D-TOF)和三维稳态构成干预序列(3D constructive interference in the steady sate,3D-CISS),明确有无肿瘤、动脉瘤等继发因素,了解血管压迫情况,如迂曲扩张的基底动脉(basilar artery,BA)和椎动脉(vertebral artery,VA),BA和(或)VA均明显扩张、延长,VA、BA的位置均出现明显偏离(图1);VA与面神经根出入脑干区(root exit zone,REZ)关系密切。确诊VBD 参考Ubogu及Zaidat提出的诊断标准。

图1 椎-基底动脉扩张延长症致面肌痉挛术前影像学表现A、B. 术前3D-TOF及3D-CISS序列轴位像,见对侧椎动脉(右侧)迂曲走行与左侧椎动脉共同位于REZ;C. 冠状位见椎基底动脉形态迂曲,位置走向异常;3D-TOF. 三维时间飞跃法血管成像序列;3D-CISS. 三维稳态构成干预序列;REZ. 面神经根出脑干区
1.3 手术方法
采用改良枕下乙状窦后入路。侧卧位,耳后发际内直切口,剪开硬膜后显露后组颅神经及其与面听神经的间隙,探查面神经REZ的责任血管,用Teflon棉将责任血管与面神经REZ隔开,如术中发现责任血管为粗大、扩张、迂曲的椎-基底动脉,张力高难以推移,难以将血管远离REZ,可采用“双面胶技术”将责任血管粘向岩骨硬脑膜,使其远离REZ,达到充分减压的目的。该技术要点是将小块明胶海绵滴上少量生物胶,形成类似双面胶的作用,然后用枪状镊子粘向责任血管,再将责任血管向颅底硬膜推过去,使二者粘合在一起,推移时间约3~5s即可。
7例中,3例行常规MVD,4例术中发现粗大的椎-基底动脉张力大,难以使用Teflon棉垫开远离REZ,故采用双面胶技术(图2),将责任血管粘向岩骨硬脑膜,同时术中注意有向脑干发出的穿支血管,术中需要特别小心保护,避免出现血管扭结,影响血供。
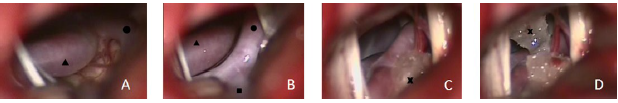
图2 椎-基底动脉扩张延长症致面肌痉挛术中表现术中采用“双面胶悬吊技术”,对侧椎动脉(▲示)位于面听神经复合体与后组颅神经之间,抬起见同侧椎动脉(●示)及同侧小脑后下动脉(■示),在面神经根出脑干区放置垫棉(×示),责任血管垫开不满意,放置带胶水的垫绵,将椎动脉粘连于岩骨硬膜
2. 结果
术后随访6个月~2年,7例均恢复良好;6例面肌抽搐症状完全消失,1例有部分残留;2例出现一过性面瘫,1例出现一过性听力下降,1例出现永久性听力下降;无复发、脑脊液漏、颅内感染、死亡。
3. 讨论
VBD临床罕见,发病率在0.06%~5.80%,确诊主要依靠影像学。Ubogu和Zaidat提出VBD的MRA半定量诊断标准:①延长,VA长度≥29.5 mm,BA 颅内段长度≥23.5 mm;②扩张,VA直径≥4.5mm;③迂曲,椎-基底动脉横向偏离超过10 mm。本文病例中,部分病例不满足上述所有条件,比如椎-基底动脉出现明显的迂曲,但VA直径没有达到标准,所以如何区分是血管的正常变异还是VBD,而且对于VBD的分期问题,类似于烟雾病的分期情况,需要进一步研究探讨。
VBD的病因尚不明确,可能是一种先天性血管异常病变,是在高血压、动脉粥样硬化等多种血管危险因素的作用下发展的结果。VBD可无任何临床症状,也可表现为严重的并发症。Wolters和Rinkel报道最常见的是缺血性卒中(17.6%),其次为脑干、颅神经压迫症状(10.3%)。VBD导致NVCS,可为任何颅神经,最常见的为第Ⅴ、Ⅶ对颅神经受压,引起TN和HFS。也可导致非典型HFS,甚至引起脑干受压症状。
Chan等发现HFS合并高血压相比无高血压病人,延髓腹外侧受压几率更高;而且,VBD可导致多组颅神经同时受压的症状,可同时出现TN、HFS、原发性高血压三种疾病。临床上,HFS常用MVD治疗。术中需注意辨认REZ,因为减压范围不足,术后疗效不佳;盲目扩大减压范围可能会带来灾难性的后果。
面神经减压范围限于REZ即可,全程减压并非必要,对于非典型HFS,除探查REZ外,还需探查垫开REZ远端压迫或接触的血管。由VBD引起的HFS,责任血管为迂曲粗大的椎-基底动脉,张力高,甚至双侧BA、VA压迫REZ,其减压术特点与常规MVD有所不同,单纯应用Teflon垫片难以推开血管,且多数为间接责任血管,直接责任血管为其深部的小脑后下动脉、小脑前下动脉及其穿支。
Shimano等报道131例HFS,33例(25%)为VA压迫,4例为双侧迂曲扩张的BA,减压手术难度较大,需要特别的技术。Han等报道12例VBD,术后出现一过性面瘫(25%),一过性听力下降(26%),永久性听力下降(8.3%)。过去对于VBD引起的HFS,由于认识不足,并发症多,手术疗效欠佳,因此有学者甚至建议对于VBD引起的颅神经疾病,不推荐行MVD。因此,在传统MVD基础上出现一些新的减压技术。有学者分别通过硬脑膜带及丝线环绕责任血管,将其悬吊在附近岩骨的硬膜上,使其远离REZ来减压。上述方法虽然可解决问题,但是对于术者手术技术要求较高,减压手术空间很小,位置深,难度较大,不易掌握。
Ichikawa等率先报道“双面胶技术”,将一种纤维蛋白粘合材料制成“双面胶带”,将其附着在血管表面,然后贴附于颞骨岩部硬脑膜,从而使责任血管远离REZ,达到减压的目的。我们也采用类似的“双面胶悬吊技术”。如果发现责任血管张力大,单纯垫开困难,就会采用该技术,其优点是操作简单,易于掌握,引起并发症的风险较低,和传统的MVD类似,可能带来的危害包括动脉损伤和无菌性脑膜炎,所以,关颅前使用含有地塞米松的生理盐水反复冲洗可使其发生率降低。
临床应用发现该方法疗效好,未见复发,对于粗大迂曲的椎-基底动脉为责任血管时,如果传统方式垫开较困难,均可使用该方法,是传统MVD的一个良好补充和改良。总之,VBD引起HFS少见,术前MRI/MRA检查了解神经血管关系十分必要,筛查VBD引起的HFS,对手术有指导意义,而不单纯理解为BA压迫面神经REZ,是一种复杂的脑血管疾病,手术治疗难度较大,采用“双面胶悬吊技术”能达到较好的疗效。
原始出处:
丁胜超,贺峰,贾继明.椎-基底动脉扩张延长症致面肌痉挛的手术治疗[J].中国临床神经外科杂志,2018(05):308-310.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#面肌痉挛#
38
#扩张#
30
#手术治疗#
34
#痉挛#
34
#基底动脉#
32