陈文明教授:多发性骨髓瘤新进展
2018-06-19 佚名 肿瘤资讯
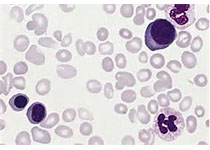
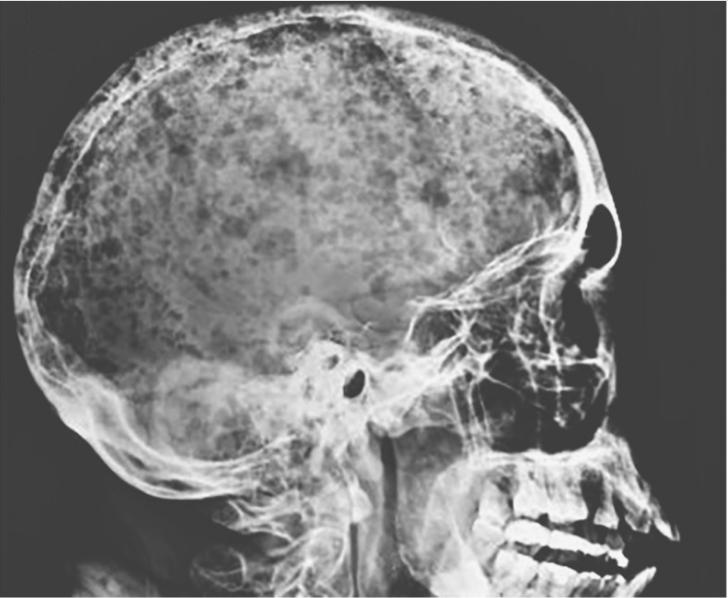
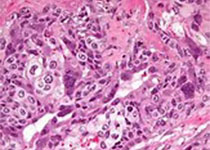
近年来,随着多种新药的出现,多发性骨髓瘤治疗的疗效显着提高,微小残留病检测也随之成为一个热点话题。目前,微小残留病的检测手段主要包括二代测序、二代流式细胞术,以及最新出现的质谱检测,这也是本次IMWG会议重点讨论的内容。质谱检测能与常规检测手段达到同样的效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
28
#陈文明#
36
好好学习天天向上
45
阅
58
学习了.长知识
0