Circulation:蛋白酶激活受体-2参与血管炎症和动脉粥样硬化的发生
2018-10-24 MedSci MedSci原创
凝血系统与血管炎症密切相关,但其机制尚不明确。近期有研究表明蛋白酶激活受体(PAR)-2是激活因子X的主要受体,在血管细胞和白细胞中均有表达,提示PAR-2可能参与炎症病理过程。现研究人员对PAR-2在血管炎症和动脉粥样硬化形成中的作用进行研究。研究人员建立了一种缺乏系统PAR-2表达的脂蛋白E缺陷的小鼠(PAR-2-/-ApoE-/-)。还通过骨髓移植建立ApoE-/- 小鼠,缺乏或仅在骨髓(B
研究人员建立了一种缺乏系统PAR-2表达的脂蛋白E缺陷的小鼠(PAR-2-/-ApoE-/-)。还通过骨髓移植建立ApoE-/- 小鼠,缺乏或仅在骨髓(BM)细胞中表达PAR-2。予以西式饮食喂养20周后,采用组织学分析、qPCR和Western blotting分析粥样硬化病损。并在体外采用BM来源的巨噬细胞来明确PAR-2的促炎症作用。此外,研究人员还在进行冠状动脉干预的患者中评估血浆激活因子X水平与冠状动脉粥样硬化的严重程度之间的相关性。
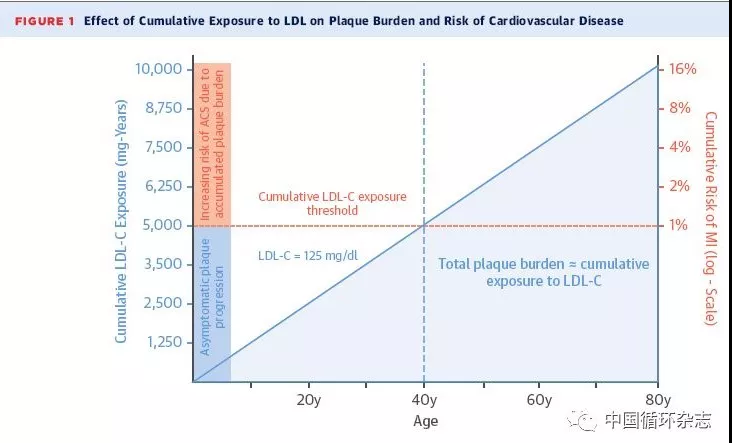
与ApoE-/-小鼠相比,PAR-2-/-ApoE-/-小鼠的动脉粥样硬化病损减少(p<0.05),伴随动脉粥样硬化斑块稳定,如脂质沉积(p<0.05)、胶原丢失(p<0.01)、巨噬细胞积累(p<0.05)以及炎症分子表达减少(p<0.05)。系统敲除ApoE-/-小鼠的PAR2可显著降低炎症分子在动脉中的表达水平。BM移植试验的结果显示造血细胞中的PAR-2可促进ApoE-/-小鼠的动脉粥样硬化。敲除PAR-2不影响代谢参数。体外试验显示激活因子X或PAR-2的特异性肽类激动剂可明显增加野生型小鼠BM来源的巨噬细胞(与PAR-2缺陷小鼠的相比)的炎症因子表达和脂质摄取。核因子κB信号激活参与PAR-2相关的血管炎症和巨噬细胞激活。在进行冠状动脉干预的人类中,血浆激活因子X的水平与冠状动脉粥样硬化的严重程度独立相关。
在ApoE-/-小鼠中,PAR-2信号激活巨噬细胞、促进血管严重,并可增加动脉粥样硬化。该信号或许也参与人类的动脉粥样硬化。
Tomoya Hara,et al.Protease-Activated Receptor-2 Plays a Critical Role in Vascular Inflammation and Atherosclerosis in Apolipoprotein E–Deficient Mice.Circulation.April 26,2018;138:1706–1719
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#蛋白酶激活受体-2#
35
#粥样硬化#
34
#蛋白酶#
47
#血管炎#
27
#血管炎症#
36
学习了谢谢分享
74
学习了谢谢
79