JAMA Neurol:院内中风患者血管内再灌注治疗率及功能预后研究
2020-09-28 MedSci原创 MedSci原创
住院脑卒中发病率呈现出上升趋势,与院外脑卒中发作相比,院内发病患者的再灌注延迟时间较长,功能预后较差
统计发现,有相当大比例的急性缺血性脑卒中发生在患者住院期间,近日研究人员评估了静脉和血管内再灌注疗法治疗住院脑卒中的时间变化趋势。

本次回顾性队列研究分析了2008年1月至2018年9月在GetWithGuidelines-Stroke国家数据库中收集的接受脑卒中治疗的患者数据,患者在院内或院外发病。研究的主要终点为血管内再灌注治疗的时间变化趋势、质量、功能结果与关键患者特征,共患病和治疗之间的关联。
在67493例住院脑卒中患者中,与仅接受静脉溶栓(平均年龄72岁,53.2%女性)的患者相比,接受血管内治疗(平均年龄69岁,49.8%女性)患者的血管危险因素发生率较高(标准化平均差>10%),但年龄或性别无显著性差异。10481例(15.5%)接受静脉溶栓治疗,2494例(3.7%)接受血管内治疗。与2008年相比,2018年住院脑卒中患者的比例增加(3.5% vs 2.7%),住院脑卒中患者使用静脉溶栓(19.1% vs 9.1%)和血管内治疗(6.4% vs 2.5%)的比例增加,其中2015年接受血管内治疗的患者比例显著增加。与接受静脉溶栓治疗的院外脑卒中患者相比,住院患者从中风识别到头颅成像(33 vs 16分钟)和溶栓治疗(81[ vs 60分钟)的中位(IQR)时间较长。调整后,与院外发病并接受静脉溶栓治疗的患者相比,接受静脉溶栓治疗的住院脑卒中患者出院后,无法独立行走、死亡或接受临终关怀(调整后的比值比为1.39)的风险增加,接受血管内治疗的住院脑卒中患者的预后也较差。
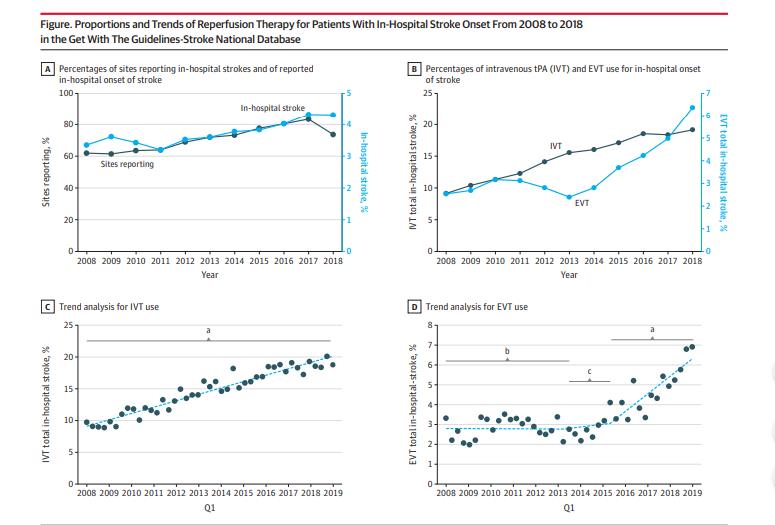
研究发现,住院脑卒中发病率呈现出上升趋势,与院外脑卒中发作相比,院内发病患者的再灌注延迟时间较长,功能预后较差。
原始出处:
Feras Akbik et al. Trends in Reperfusion Therapy for In-Hospital Ischemic Stroke in the Endovascular Therapy Era.JAMA Neurol. September 21, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
27
学习
61
考虑到非标准化的疾病标准,应考虑进一步设计良好的前瞻性试验以证实这些结果。
83
#再灌注治疗#
43
#功能预后#
39
#中风患者#
38
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
48
中风是俗称,应该称为缺血性卒中吧
52