JAMA ONCOL:造血干细胞移植后继发实体瘤患者预后评估
2018-11-29 MedSci MedSci原创
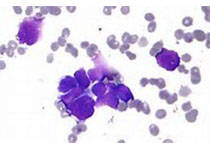
已有充分的临床记录证明造血干细胞移植(HSCT)后会发生继发实体瘤(SSCs)。然而,HSCT后发生SSC的患者的临床预后数据有限。JAMA ONCOL近期发表了一篇文章,评估HSCT后发生SSC患者的预后。
已有充分的临床记录证明造血干细胞移植(HSCT)后会发生继发实体瘤(SSCs)。然而,HSCT后发生SSC的患者的临床预后数据有限。JAMA ONCOL近期发表了一篇文章,评估HSCT后发生SSC患者的预后。
该研究使用了来自26个国家的4065名患者的数据,包括18种不同癌症的患者。数据分析于2017年9月3日至2018年3月17日进行。主要研究结果包括总生存,死亡原因等。共有220 617例患者接受了移植手术,其中4065例(1.8%)出现HSCT后继发实体瘤的患者纳入研究。在4065例患者中,2321例(57.1%)为男性,1744例(42.9%)为女性,诊断为继发实体瘤的平均年龄为59.1岁。5年总生存率为47%。胰腺癌,肺癌,肝胆癌,食管癌,脑癌和胃癌的SSC诊断后5年总生存率较差,中位生存期为0.6至1年。子宫内膜癌,结肠直肠癌,肉瘤,卵巢癌,膀胱癌,口咽癌和肾癌的5年总生存率中等,中位生存期为2至10年。黑色素瘤,乳腺癌,前列腺癌,子宫颈癌和甲状腺癌的5年总生存率较优,中位生存期为10年或更长。共有1777名患者(43.7%)死亡,其中1256名(74.8%)死于SSC,344名(20.5%)死于原发病,79名(4.7%)死于其他原因。
原始出处:
André Tichelli, Eric Beohou, et al. Evaluation of Second Solid Cancers After Hematopoietic Stem Cell Transplantation in European Patients. JAMA ONCOL. November 2018 doi:10.1001/jamaoncol.2018.4934
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#预后评估#
43
#继发#
27
#患者预后#
31
#细胞移植#
32
#Oncol#
21
#造血干细胞#
26
#造血#
28
学习了
50