Cancer:前列腺癌活检格林森评分9到10患者的前列腺特异性抗原水平和前列腺癌特异性死亡风险
2021-06-23 AlexYang MedSci原创
前列腺特异性抗原(PSA)是一种由前列腺上皮细胞表达的糖蛋白,是前列腺癌(PC)治疗前和治疗后的重要预后标志物。研究表明,诊断前PSA迅速增加与复发、转移和PC特异性死亡的风险增加有关。
前列腺特异性抗原(PSA)是一种由前列腺上皮细胞表达的糖蛋白,是前列腺癌(PC)治疗前和治疗后的重要预后标志物。研究表明,诊断前PSA迅速增加与复发、转移和PC特异性死亡的风险增加有关。

对于前列腺特异性抗原(PSA)水平≤4 ng/mL(vs >4 ng/mL)且Gleason评分(GS)为9至10分的男性,如何确定超出常规临床实践的工作,以改善其治疗效果仍有待确定。
在1992年2月25日至2016年2月25日期间,17632名临床T1-4级PC且活检GS为6至10的男性在一个学术中心接受了根治性前列腺切除术。研究人员使用了多变量Fine和Gray回归来评估前列腺癌特异性死亡(PCSM)的风险,用交互模型评估了PSA≤4纳克/毫升与PSA>4纳克/毫升在活检GS为9至10与≤8的男性中的预后意义,除了已知的PC预后因素外,还对辅助和/或挽救性放疗和雄性激素阻断疗法(ADT)的使用进行了时间依赖的调整。
结果发现,在活检GS为9至10的男性与≤8的男性,以及PSA水平≤4纳克/毫升与>4纳克/毫升的男性中,存在着显著的相互作用(调整后的危险比[AHR],2.87;95%置信区间[CI],1.02-8.08;P=046)。具体而言,在活检GS为9至10且PSA水平≤4纳克/毫升与>4纳克/毫升的男性中,PCSM的比率明显较高(AHR,2.59;95%CI,1.19-5.67;P=0.017);然而,在活检GS≤8且PSA水平≤4 ng/ml与>4 ng/ml的男性中,PCSM的风险没有明显差异(AHR,0.90;95%CI,0.46-1.78;P=0.771)。此外,术后使用ADT的时间也与PCSM的风险增加有关(AHR,10.76;95%CI,6.88-16.81;P<0.0001)。
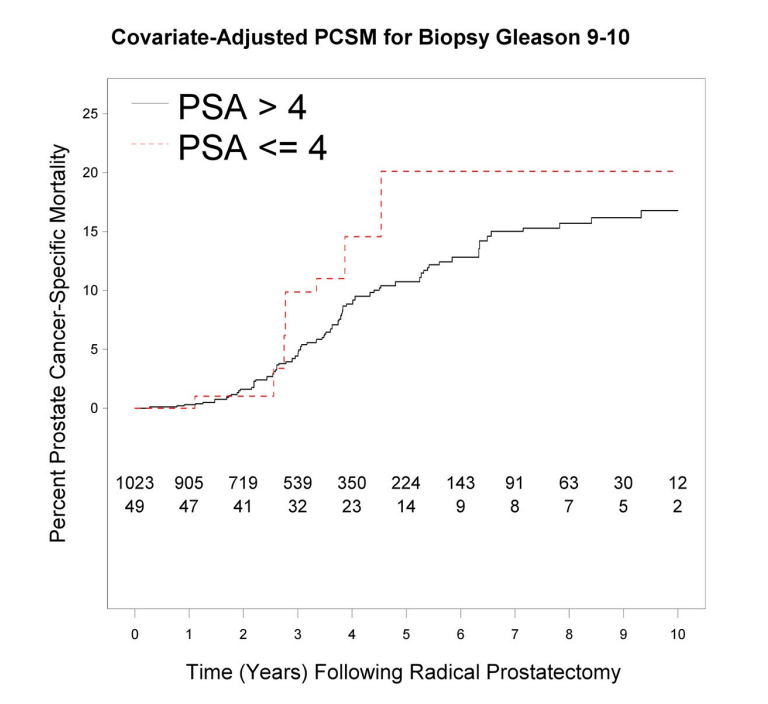
活检格林森评分9到10患者的PCSM
综上所述,一些PSA≤4纳克/毫升且活检GS为9至10的男性可能有病理或遗传变异,使他们用目前的护理标准难以治愈。应考虑进行额外的小细胞、神经内分泌和遗传变异评估工作。
原始出处:
Daniel W Kim, Ming-Hui Chen, Jing Wu et al. Prostate-specific antigen levels of ≤4 and >4 ng/mL and risk of prostate cancer-specific mortality in men with biopsy Gleason score 9 to 10 prostate cancer. Cancer. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#前列腺特异性抗原#
35
#特异性#
35
#特异性抗原#
41
#格林森评分#
54
#死亡风险#
0
#活检#
42
#抗原#
31
前列腺癌相关研究,学习了,谢谢梅斯
66