J Neurointerv Surg:急性脑梗死,支架取栓器VS直接血栓抽吸哪个效果更好?
2020-11-12 MedSci原创 MedSci原创
“首通效应”(FPE)最初是用支架取出器描述的,指的是在一次装置通过后,在没有救援治疗的情况下获得的(近乎)完全的血管重建,并与改善临床结果和降低死亡率有关。本研究报告了抽吸与
“首通效应”(FPE)最初是用支架取出器描述的,指的是在一次装置通过后,在没有救援治疗的情况下获得的(近乎)完全的血管重建,并与改善临床结果和降低死亡率有关。本研究报告了抽吸与支架取栓器(ASTER)试验中的FPE率和效益,研究结果已在线发表于J Neurointerv Surg。

ASTER是一项随机试验,目的在于:比较血管造影血管重建与支架取栓器(SR)和直接血栓抽吸(CA)血栓切除术的效果,由外部核心实验室使用改良的脑梗死溶栓(mTICI)量表评估;比较SR和CA技术治疗的患者之间的FPE率(由mTICI 2c/3定义,单次通过后无抢救治疗);比较FPE-SR和FPE-CA患者之间的结果,以及FPE和非FPE患者之间的结果。
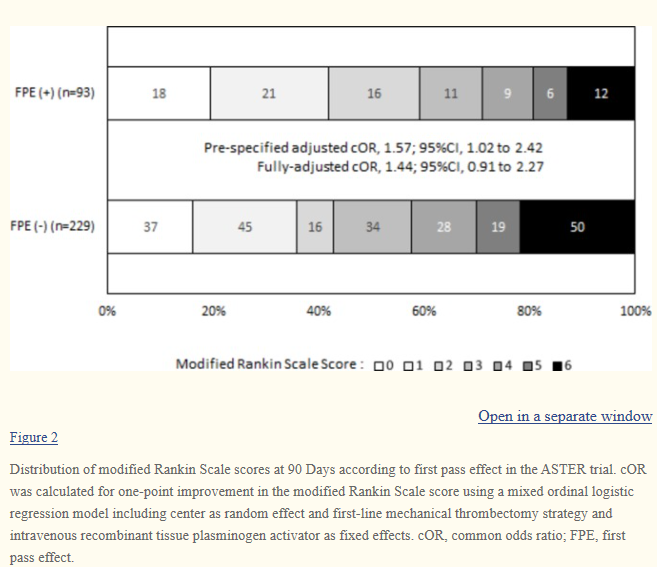
结果,97/336名患者实现了FPE(28.9%),SR和CA之间无显著差异(分别为53/169名患者(31.3%)vs 44/167名患者(26.3%),CA与SR的校正RR为0.84,95%CI 0.54~1.31;P=0.44)。在对分配臂和随机分层因素进行预设校正后,患者的FPE与临床结果显著改善和死亡率降低相关,出血性转化和手术并发症的发生率显著低于非FPE患者。
综上所述,该研究结果表明,在ASTER试验中,SR和CA的FPE率相似,FPE与显著改善的结果相关。有必要采用新的技术和设备来提高FPE的比率。
原始出处:
Célina Ducroux, Michel Piotin, et al., First pass effect with contact aspiration and stent retrievers in the Aspiration versus Stent Retriever (ASTER) trial. J Neurointerv Surg . 2020 Apr;12(4):386-391. doi: 10.1136/neurintsurg-2019-015215. Epub 2019 Aug 30.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血栓抽吸#
48
了解
60
#脑梗#
42
#取栓#
35
已读
71
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
45
好文章,学习了
54