ARD:调节性 T 细胞功能障碍作为巨细胞动脉炎治疗靶点的新发现
2022-02-03 MedSci原创 MedSci原创
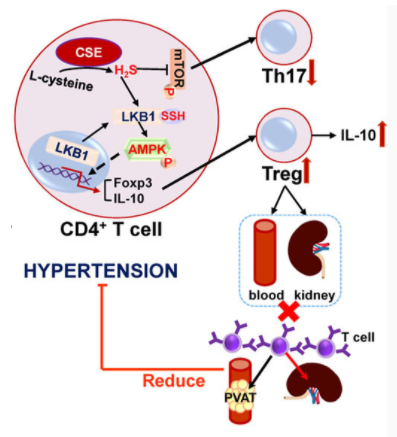
低糖酵解和钙信号传导是巨细胞动脉炎中 Treg 细胞功能障碍和炎症的原因。
目的:巨细胞动脉炎(GCA)是最常见的系统性血管炎,影响老年人,发病高峰期在 70-80 岁之间。GCA 通常涉及主动脉和/或其大口径分支。促炎性CD4+ T辅助细胞亚群(即Th1和Th17细胞)和调节性T细胞 (Tregs,FOXP3对Treg分化和功能必不可少) 之间的不平衡被认为与 GCA 的发病机制有关,并且 Treg 功能障碍与活动性疾病有关。该研究工作旨在探索 Treg 功能障碍的病因及其受缓解诱导免疫调节治疗影响的方式。
方法:共有 41 名 GCA 患者被分为活动性疾病 (n=14) 和缓解期疾病 (n=27)。 分离出GCA 患者和健康献血者 (HD) 的外周血单核细胞(PBMC)并采用流式分选出CD4+CD25highCD127lo Treg细胞,进行RNA-seq转录组分析和表型分析(包括流式细胞术、钙流实验和Treg抑制实验)。
结果:转录组分析揭示了 27 个基因,这些基因在 GCA 衍生和 HD 衍生的 Treg 之间受到差异调节。其中,研究者鉴定出了转录因子、糖酵解酶和 IL-2 信号传导介质。证实了叉头盒 P3 (FOXP3) 和干扰素调节因子 4 (IRF4) 在蛋白质水平上的下调,并确定了糖蛋白 A 重复优势 (GARP) 和 CD25的无效诱导,以及减少的 T 细胞受体 (TCR) 诱导的钙内流与 GCA 中 Treg 功能障碍的相关性。 HD 衍生的 Treg 中糖酵解的抑制复制出了 GCA Treg的大多数已识别功能障碍,表明糖酵解酶下调的中心致病作用。对托珠单抗治疗患者亚组的单独分析确定了TCR 诱导的钙内流和 Treg抑制功能的恢复与疾病缓解有关。
结论:以上研究结果表明,低糖酵解和钙信号传导是巨细胞动脉炎中 Treg 细胞功能障碍和炎症的原因。
出处:
Adriawan IR, Atschekzei F, Dittrich-Breiholz O, et al. Novel aspects of regulatory T cell dysfunction as a therapeutic target in giant cell arteritis. Annals of the Rheumatic Diseases 2022;81:124-131.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#治疗靶点#
52
#动脉炎#
55
#新发现#
45
#功能障碍#
40
#巨细胞#
53
#细胞功能#
32