盘点:近期有关哮喘相关疾病研究进展
2016-11-06 MedSci MedSci原创
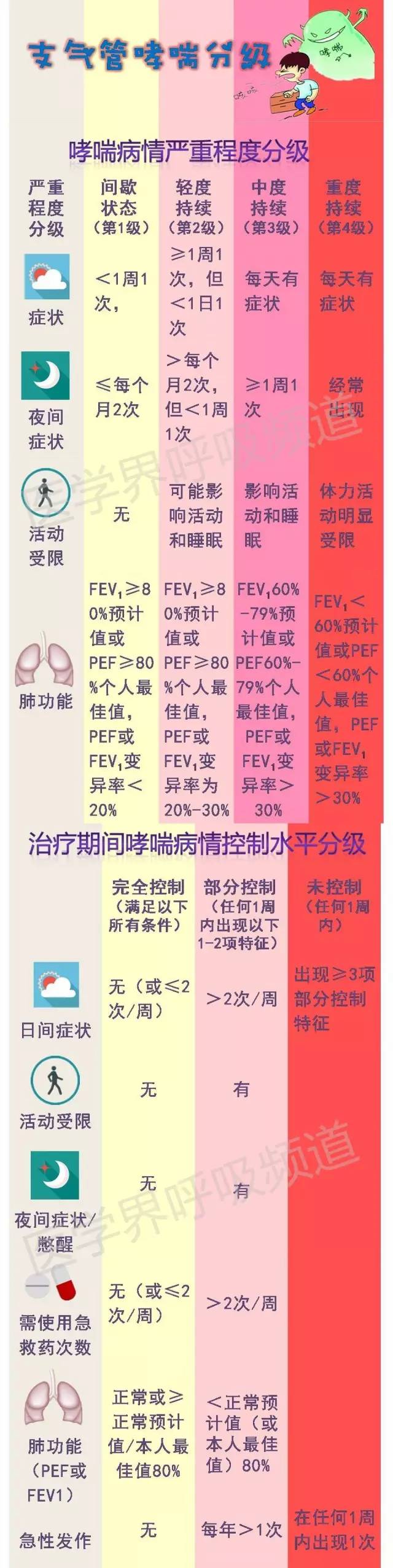
哮喘又名支气管哮喘。支气管哮喘是由多种细胞及细胞组分参与的慢性气道炎症,此种炎症常伴随引起气道反应性增高,导致反复发作的喘息、气促、胸闷和(或)咳嗽等症状,多在夜间和(或)凌晨发生,此类症状常伴有广泛而多变的气流阻塞,可以自行或通过治疗而逆转。本文梅斯医学小编为您盘点近期哮喘治疗相关进展,与大家分享学习。【1】Allergy:变应性过敏在哮喘病儿童患者中发病率很高来自伦敦的Annica Öne
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病研究#
41
#研究进展#
32
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
53
谢谢分享学习
47
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
53
谢谢分享学习
51
分享。谢谢谢谢。注意很久。
0
学习新知识!
32
学习啦!!!
24