Hypertension:青少年动脉僵硬度可反向增加其肥胖和高血压风险!
2021-12-24 Nebula MedSci原创
全球青少年和年轻人肥胖和高血压的发生率均与日俱增。虽然肥胖、血压 (BP) 升高和高血压是动脉硬化和颈动脉内膜-中膜厚度 (cIMT) 的公认的危险因素,还是颈动脉粥样硬化心血管疾病的替代标志物,但在
全球青少年和年轻人肥胖和高血压的发生率均与日俱增。虽然肥胖、血压 (BP) 升高和高血压是动脉硬化和颈动脉内膜-中膜厚度 (cIMT) 的公认的危险因素,还是颈动脉粥样硬化心血管疾病的替代标志物,但在青少年和年轻人中,这些因素的时间或双向关系尚不明确。
近日,发表在《高血压》上的一项交叉滞后队列研究,评估了颈动脉-股动脉脉搏波速度 (cfPWV,动脉硬度的一种测量方法) 和颈动脉内膜-中膜厚度与超重/肥胖和血压升高/高血压的时间纵向相关性。
纳入了来自 Avon父母和儿童纵向研究的 3862 位 17.7 岁的青少年,随访了 7 年。采用超声评估 cfPWV 和 cIMT。通过双能 X 线吸收测定法评估总脂肪量和躯干脂肪量以及瘦体重。使用逻辑回归、线性混合效应和交叉滞后结构方程模型分析数据,并进行协变量校正。
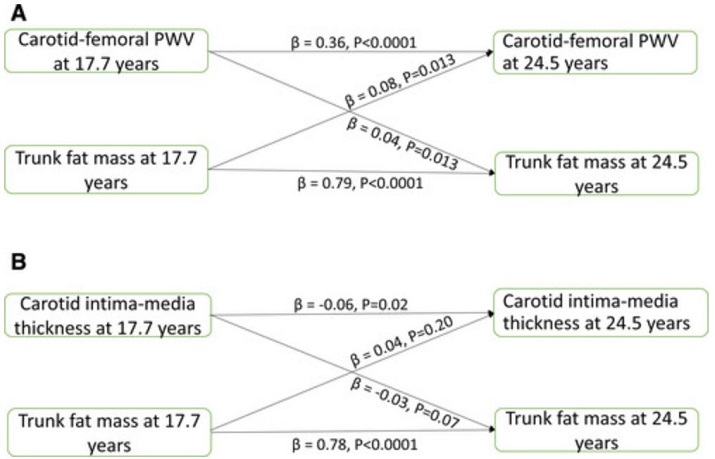
动脉测量值和体脂之间的时间因果关系
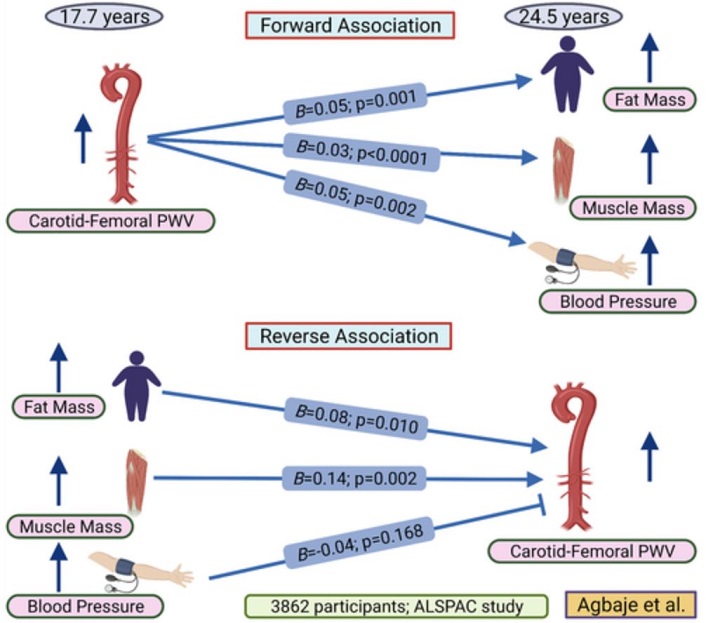
受试者包括 1719 名男生和 2143 名女生。17.7 岁时高 cfPWV 与24.5 岁时的收缩压升高/高血压(优势比 1.20[1.02-1.41];p=0.026)、舒张压升高/高血压(1.77 [1.32–2.38]; p<0.0001)、体重指数-超重/肥胖(1.19 [1.01–1.41]; p=0.041)和躯干脂肪量超重/肥胖(1.24 [1.03–1.49]; p=0.023)风险相关。而且,cfPWV 进展与 7 年内收缩压和舒张压升高直接相关(分别是 16 mmHg 和 28 mmHg;p均<0.0001)。
动脉测量值和血压之间的时间因果关系
但是,17.7 岁时高 cIMT 与随访过程中的肥胖和血压升高风险无关。不过,cIMT 进展却与所有肥胖指标和舒张压升高直接相关。
在时间分析中,基线 cfPWV 与随访过程中的收缩压和舒张压直接相关,但是,基线血压与随访过程中 cfPWV 的变化无关。 cfPWV与肥胖具有双向的相关性,但 cIMT 无此双向相关性。
动脉僵硬度与肥胖和高血压的相关性总结示意图
综上,从青春期即开始预防肥胖和高血压,可能需要同时注意控制动脉僵硬度。
原始出处:
Andrew O. Agbaje, et al. Effects of Arterial Stiffness and Carotid Intima-Media Thickness Progression on the Risk of Overweight/Obesity and Elevated Blood Pressure/Hypertension: a Cross-Lagged Cohort Study. Hypertension. 2022;79:159–169
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#TENS#
42
#PE#
50
#Hypertension#
46
#动脉僵硬#
52
#动脉僵硬度#
51