Cell:世界首例神经疾病模型猪诞生 推动阿尔兹海默症等疾病治疗
2018-03-31 王莹 人民网
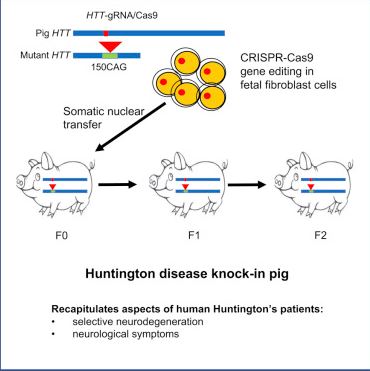
记者从中国科学院获悉,经过四年努力,广东科学家领衔的国际研究团队首次利用基因编辑技术(CRISPR/Cas9)和体细胞核移植技术,成功培育出世界首例亨廷顿舞蹈病基因敲入猪。它能精准模拟出人类神经退行性疾病,为治疗亨廷顿舞蹈病、老年痴呆等疾病提供稳定、可靠的动物模型,推动药物筛选和治疗方案制定。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
34
#疾病模型#
45
#疾病治疗#
21
#世界首例#
0
#Cell#
26
学习一下谢谢分享
32
#阿尔兹海默#
26
#猪#
25
#神经疾病#
36
学习了
45