Sleep Med:长期CPAP改善中度-重度OSA高龄患者生存
2015-11-26 MedSci MedSci原创
西班牙马德里12 de Octubre大学医院呼吸科Daniel López-Padilla和同事研究持续正压通气与患中度-重度阻塞性睡眠呼吸暂停的老年人的生存的关系。研究结果2015年11月23日在Sleep Medicine在线发表。目标:现有证据表明长期CPAP( continuous positive airway pressure ,持续气道正压)对OSA(obstructive sle
西班牙马德里12 de Octubre大学医院呼吸科Daniel López-Padilla和同事研究持续正压通气与患中度-重度阻塞性睡眠呼吸暂停的老年人的生存的关系。研究结果2015年11月23日在Sleep Medicine在线发表。
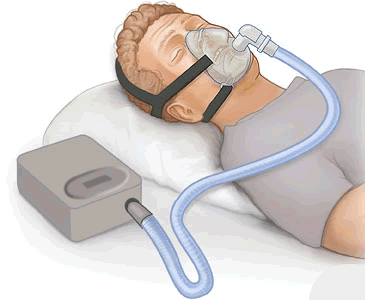
目标:现有证据表明长期CPAP( continuous positive airway pressure ,持续气道正压)对OSA(obstructive sleep apnea,阻塞性睡眠呼吸暂停)老年患者的生存有有益影响,通常年龄截值在60到70岁之间。研究目标是确定长期CPAP对OSA高龄患者(例如≥80岁的老年人)的影响。
方法:观察性研究长期CPAP对中度到重度OSA(低通气指数≥20)的高龄人群历史队列生存的影响。将受试者分成两组:试验组进行标准CPAP治疗(每晚≥4小时),对照组没有进行CPAP治疗。使用Kaplan–Meier曲线和Cox模型生存分析确定长期CPAP与OSA高龄患者更长生存之间的关联。
结果:研究共纳入155例高龄受试者(84名男性和71名女性,平均年龄为81.5±1.5岁),随访53个月(四分位范围,41 - 77个月),共有83人死亡。
CPAP组包含132名受试者,79名(60%)受试者坚持观察。Kaplan–Meier曲线显示与对照组相比(52个月,95%CI 41-64),试验组生存期较长(91个月,95%CI 76-106),差别具有统计学意义(log-rank 16.9,P<0.0001)。
虽然受试者卒中史与高死亡率显著相关(HR 2.18,95%CI 1.14-4.17,P=0.02),调整后Cox分析显示CPAP治疗与更高的生存率相关(HR=0.46,95%CI 0.27-0.78,P=0.004)。
结论:长期CPAP治疗可能与中度-重度OSA高龄患者生存期更长相关。
原始出处:
Daniel López-Padilla, Rodrigo Alonso-Moralejo, Miguel Ángel Martínez-García, et all. Continuous positive airway pressure and survival of very elderly persons with moderate to severe obstructive sleep apnea. Sleep Medicine. Available online 23 November 2015.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PAP#
33
#患者生存#
30
#长期CPAP#
27
继续努力
102
继续研究
127
支持一下
51
大有帮助
98
好好好学习
114
#高龄患者#
36
#CPAP#
30