Stroke:心脏计算机断层扫描与经食管超声心动图检测左心耳血栓效果比较
2021-11-21 MedSci原创 MedSci原创
具有延迟成像的心脏计算机断层扫描是TEE可靠的替代方案。它可以使患者和医疗保健人员免于接受过多的TEE检查。
左心耳(LAA)血栓可能出现在导致左心房血流停滞的情况下,尤其是在心房颤动中,是心源性卒中的重要来源。根据2项大型前瞻性研究,经食道超声心动图(TEE)目前被认为是检测LAA血栓的金标准。然而,TEE是一种半侵入性且耗时的手术,并且TEE有时可能会引起不适并出现并发症。因此,心脏计算机断层扫描已被广泛用于LAA血栓的检测。
近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员进行了系统回顾和荟萃分析,以评估与TEE相比,心脏计算机断层扫描对LAA血栓检测的诊断准确性水平。
从1977年1月到2021年2月,研究人员对PubMed、Embase和Cochrane图书馆数据库进行了全面检索,纳入了与TEE相比,评估心脏计算机断层扫描对LAA血栓的诊断准确性的研究。研究人员使用双变量随机效应模型计算了LAA血栓的敏感性、特异性和后验概率。诊断准确性研究的质量评估-2工具用于质量评估。
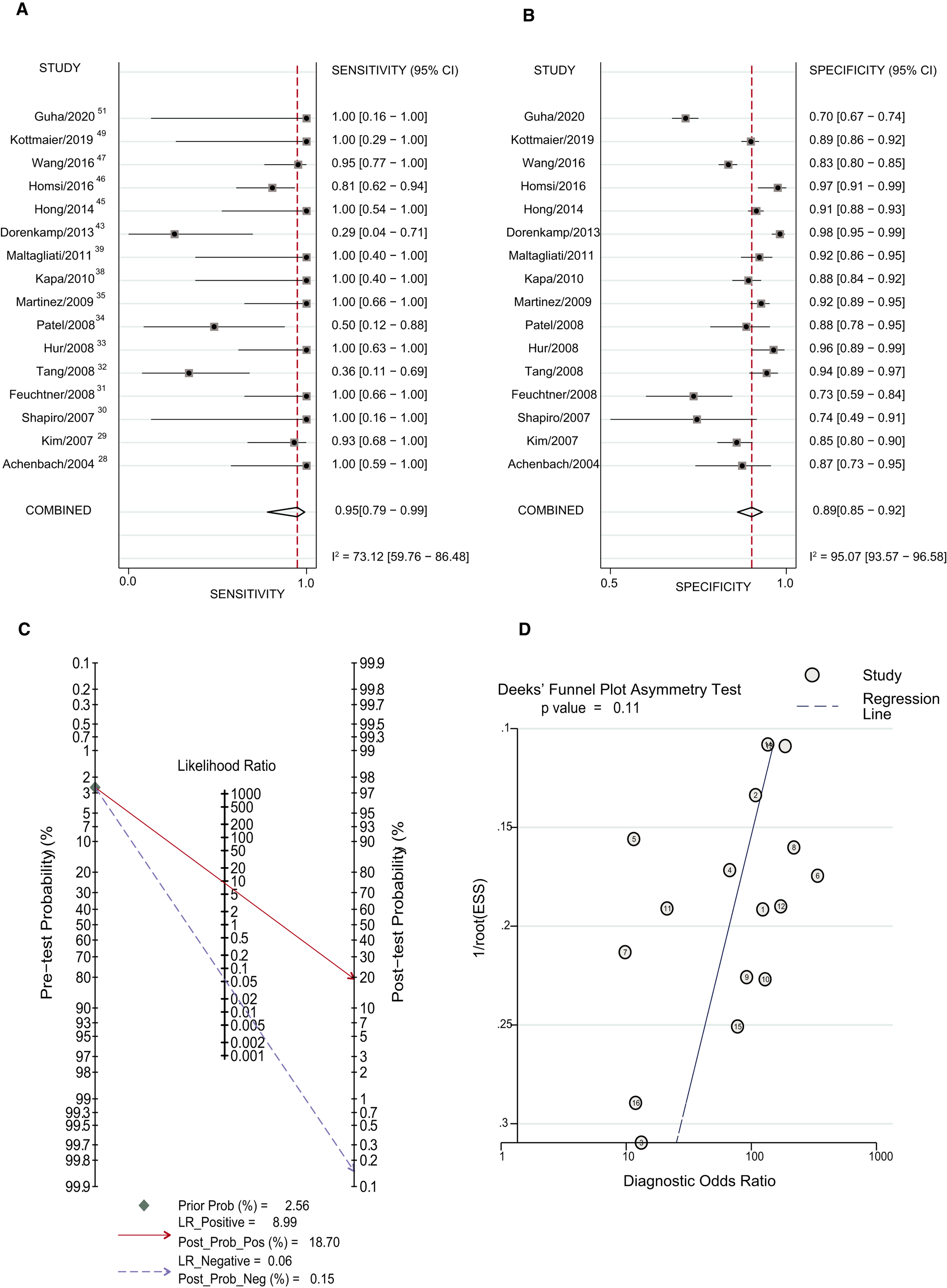
该研究共纳入了27项研究,涉及了6960名患者。早期影像学研究的总体敏感性为0.95(95%CI为0.79-0.99),特异性为0.89(95%CI为0.85-0.92)。正后验概率为19.11%,负后验概率为0.16%。延迟成像研究的总体敏感性为0.98(95%CI为0.92-1.00),特异性为1.00(95%CI为0.98-1.00)。正后验概率为95.76%,负后验概率为0.12%。延迟成像方法显著提高了特异性(1.00 vs. 0.89;P<0.05)和阳性后验概率(95.76% vs. 19.11%;P<0.05)。
由此可见,具有延迟成像的心脏计算机断层扫描是TEE可靠的替代方案。它可以使患者和医疗保健人员免于接受过多的TEE检查。
原始出处:
Shandong Yu.et al.Cardiac Computed Tomography Versus Transesophageal Echocardiography for the Detection of Left Atrial Appendage Thrombus: A Systemic Review and Meta‐Analysis.stroke.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.022505
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#心动图#
57
非常好的研究,患者往往因为不能耐受tee而不愿意检查
55
#超声心动图#
60
#计算机#
45
#食管#
30
#左心耳#
44
学习了
53
好极了
51