Mol Neurobiol:新研究为对抗恶性脑瘤提供新希望
2016-09-28 佚名 生物谷
英国南安普敦大学的研究人员最近发现一种阻止胶质母细胞瘤扩散的新方法。胶质母细胞瘤是成年人中最常见并且最具侵袭性的一种恶性脑瘤,这种疾病具有生长快速易于扩散的特点。胶质母细胞瘤细胞会向脑的其他部分延伸,导致想要将其彻底移除变得非常困难。 虽然科学家们已经在白血病和其他一些癌症治疗方面取得了巨大进展,但是对于胶质母细胞瘤如何形成以及肿瘤细胞如何侵入脑组织仍然了解较少。 在这篇发表在国际学术

英国南安普敦大学的研究人员最近发现一种阻止胶质母细胞瘤扩散的新方法。胶质母细胞瘤是成年人中最常见并且最具侵袭性的一种恶性脑瘤,这种疾病具有生长快速易于扩散的特点。胶质母细胞瘤细胞会向脑的其他部分延伸,导致想要将其彻底移除变得非常困难。
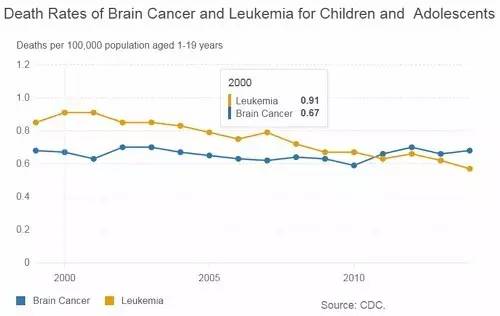
虽然科学家们已经在白血病和其他一些癌症治疗方面取得了巨大进展,但是对于胶质母细胞瘤如何形成以及肿瘤细胞如何侵入脑组织仍然了解较少。
在这篇发表在国际学术期刊Molecular Neurobiology上的文章中,Dr. Elodie Siney在Dr. Sandrine Willaime-Morawek的指导下,对一类叫做ADAM的酶进行了分析,研究这类酶如何影响人类肿瘤细胞的运动和功能。
研究结果表明如果能够阻断ADAM10和ADAM17这两个酶的作用,肿瘤细胞就会停止生长和迁移,甚至可以通过传统的癌症治疗方法,包括放疗、化疗和手术将癌细胞从生长位置清除。
研究人员表示:“如果这些结果能够在胶质母细胞瘤的动物模型上得到证实,这项发现将对病人和医生来说变得特别重要。胶质母细胞瘤是一种灾难性疾病,通常不可治愈。我们发现阻断ADAM的作用有望抑制肿瘤生长降低传统治疗之后的复发风险,提高手术完全移除肿瘤的机会,提高病人生存率。”
原始出处:
Elodie J. Siney, Alexander Holden, Elizabeth Casselden, Harry Bulstrode, Gareth J. Thomas, Sandrine Willaime-Morawek.Metalloproteinases ADAM10 and ADAM17 Mediate Migration and Differentiation in Glioblastoma Sphere-Forming Cells.Molecular Neurobiology DOI: 10.1007/s12035-016-0053-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#恶性脑瘤#
32
#新希望#
31
#Bio#
31
#Biol#
30
#脑瘤#
37