Br J Cancer:药用级别IgG削弱奥沙利铂对结肠癌细胞的抗癌活性
2021-02-15 xiaozeng MedSci原创
奥沙利铂(Oxaliplatin)作为第三代铂类抗癌药。相比于其他铂衍生物(如顺铂和卡铂),奥沙利铂的胺基被二氨基环己烷所取代,从而可以更快更有效地抑制DNA的合成。
奥沙利铂(Oxaliplatin)作为第三代铂类抗癌药。相比于其他铂衍生物(如顺铂和卡铂),奥沙利铂的胺基被二氨基环己烷所取代,从而可以更快更有效地抑制DNA的合成。
既往的临床前研究显示,在结肠癌中,奥沙利铂与5-氟尿嘧啶(5-fluorouracil)联合使用可以产生协同抗癌作用。而在临床上,在5-氟尿嘧啶和亚叶酸(甲酰四氢叶酸,leucovorin)(FOLFOX方案)治疗组合中添加奥沙利铂可显着提高结肠癌患者的生存率,而含奥沙利铂的治疗方案已成为结肠癌的一个治疗标准。
免疫球蛋白G(IgG)是血浆B细胞产生和分泌的一种最常见的抗体类型。在临床实践中,IgG的补充特别有益于炎症性疾病患者。由于炎症已被认为是癌症发生发展的新兴标志,因此越来越多的临床试验试图评估抗炎策略在癌症治疗中的益处。
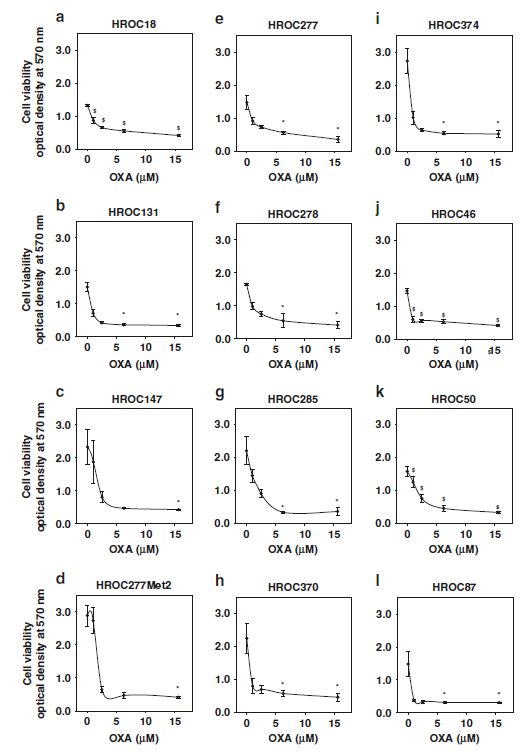
奥沙利铂抑制结肠癌细胞的活力
既往研究显示,细胞毒性化疗会损害免疫系统功能,直至出现严重的免疫缺陷。某些癌症患者可能需要通过补充IgG来弥补后者的发生。最近的证据证实静脉注射IgG会损害癌细胞的生存能力,然而,目前尚无相关研究评估IgG是否有益于接受化疗的癌症患者。
该研究旨在探究药用级别人源IgG对于一系列患者来源的有/无化学干预的结肠癌细胞系的活力的影响。通过流式细胞仪分析细胞死亡作用。此外,研究人员在蛋白水平上评估了奥沙利铂和IgG对ERK1/2信号通路的影响。
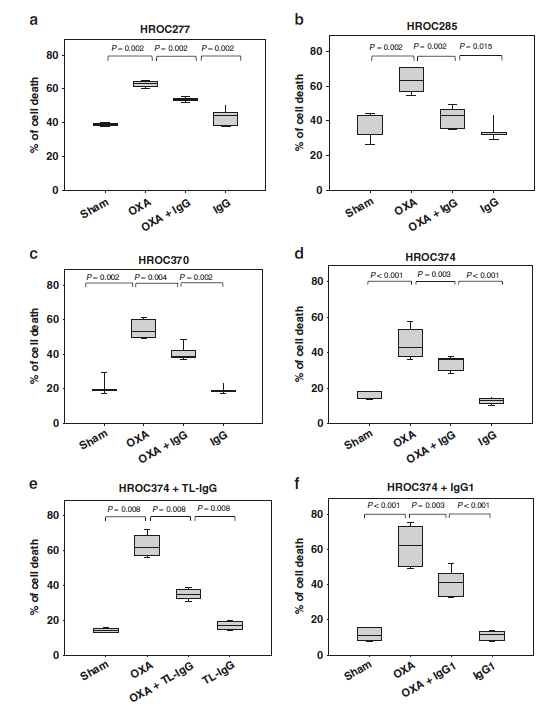
药用级别IgG减少奥沙利铂诱导的细胞死亡
通过评估药用级别IgG(如PRIVIGEN®IgG和Tonglu®IgG)与化学疗法的联合作用,研究人员并没有直接观察到IgG对肿瘤细胞生存力的任何显著影响。然而,研究人员发现IgG能够显著的损害奥沙利铂的抗肿瘤作用。原发癌细胞系能够表达IgG受体并在细胞内积累IgG。此外,尽管奥沙利铂能诱导ERK1/2的活化,相反的,IgG会抑制ERK1/2的活性。
总而言之,该研究结果显示,药用级别IgG可以削弱奥沙利铂的抗癌活性。这些数据也强烈表明,治疗性IgG作为联合用药可能会对癌症患者产生一些有害的副作用。这些临床前观察结果也为进一步的临床前研究以及流行病学和临床研究奠定了一定的基础。
原始出处:
Shang, Y., Zhang, X., Lu, L. et al. Pharmaceutical immunoglobulin G impairs anti-carcinoma activity of oxaliplatin in colon cancer cells. Br J Cancer (09 February 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#铂#
23
#癌细胞#
27
#IgG#
33
涨知识
67