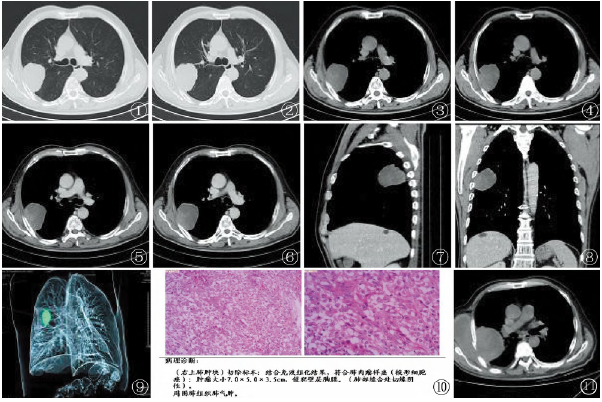
原发性肺肉瘤样癌的CT表现与鉴别诊断
2019-10-14 卢跃忠 唐向利 吴英哲 医学影像学杂志
原发性肺肉瘤样癌(PSC)是一种非常少见的、具有较高侵袭性的肺恶性上皮肿瘤,其发病率低侵袭性强,预后差,术后易复发,临床表现无特异性。在2015年WHO肺肿瘤的分类中主要包括了5种亚型代表其形态学谱系:多形性癌(pleomorphic carcinoma,PC),梭形细胞癌(spindle cell carcinoma,SCC),巨细胞癌(giant cell carcinoma,GCC),癌肉瘤
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











已读
49
#原发性#
25
#肉瘤样癌#
45
#鉴别诊断#
23
#CT表现#
39
#肺肉瘤样癌#
27