NEJM:内镜或开放静脉移植物采集对冠状动脉旁路移植术的影响
2019-01-10 xing.T MedSci原创
由此可见,在接受CABG的患者中,研究人员未发现开放性静脉移植物采集和内镜下静脉移植物采集对主要心脏不良事件风险的影响存在显著差异。
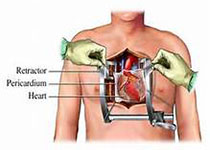
隐静脉移植是冠状动脉旁路移植术(CABG)最常用的移植血管。静脉移植物采集技术对长期临床结具的影响尚未得到很好的归纳总结。
近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员在16个退伍军人事务心脏外科中心随机分配接受CABG的患者进行开腹或内窥镜静脉移植物采集。该研究的主要结局是主要不良心脏事件的复合结局,包括任何原因导致的死亡、非致死性心肌梗死和重复血运重建。还评估了腿部伤口并发症。
该研究共纳入了1150名患者接受了随机分组。在中位随访2.78年,主要结局在开放组有89名患者(15.5%),在内镜组有80名患者(13.9%)(风险比为1.12; 95%置信区间[CI]为0.83-1.51; P=0.47)。开放组共46名患者(8.0%)和内镜组37名患者(6.4%)死亡(风险比为1.25; 95%CI为0.81-1.92); 开放组34例(5.9%)患者发生心肌梗死,内镜组27例(4.7%)患者(风险比为1.27; 95%CI为0.77-2.11)死亡,开放组35例(6.1%)和内镜组31例(5.4%)患者发生血运重建(风险比为1.14; 95%CI为0.70-1.85)。开放组中18名患者(3.1%)和内镜组中8名患者(1.4%)发生腿部伤口感染(相对风险为2.26; 95%CI为0.99-5.15)。
由此可见,在接受CABG的患者中,研究人员未发现开放性静脉移植物采集和内镜下静脉移植物采集对主要心脏不良事件风险的影响存在显著差异。
原始出处:
Marco A. Zenati,et al.Randomized Trial of Endoscopic or Open Vein-Graft Harvesting for Coronary-Artery Bypass.NEJM.2019.https://www.nejm.org/doi/full/10.1056/NEJMoa1812390
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉移植物采集#
28
#静脉#
26
#植物#
32
#移植术#
35
#旁路移植术#
35
#内镜#
28
#冠状动脉旁路移植术#
41
#移植物#
26