Arthritis Rheumatol:多关节幼年特发性关节炎早期开始使用生物制剂有帮助吗?
2021-10-08 MedSci原创 MedSci原创
在未经治疗的多关节JIA受试者中,在基线评估的3个月内开始 bDMARDs与更快实现非活动性疾病相关。这些结果证明了病程轨迹分析作为确定治疗效果的一种方法。
研究目的:研究早期使用改善疾病的抗风湿生物制剂(bDMARDs) 对未经治疗的多关节幼年特发性关节炎 (JIA) 病程的影响。
方法:研究者分析了参与多关节JIA开始时间优化研究(STOP-JIA) 中的多关节JIA患者(n = 400)和一个来自儿童关节炎和风湿病研究联盟登记处的比较队列(n = 248)的数据。潜在类轨迹建模(LCTM)应用于根据从基线开始12个月内的疾病活动(临床幼年关节炎10个关节的疾病活动评分)确定具有不同病程的患者亚组。
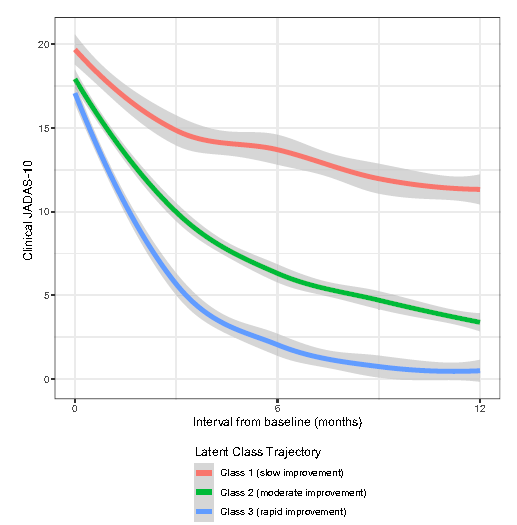
结果:在STOP-JIA研究中,198名受试者(49.5%)在基线评估的3个月内接受了 bDMARDs。LCTM分析生成了3个潜在类别,代表3个不同的疾病轨迹,其特征是随着时间的推移疾病活动缓慢、中度或迅速改善。快速改善轨迹中的受试者从基线开始的6个月内获得非活动性疾病。在调整人口统计学特征、临床属性和基线疾病活动性之后发现接受bDMARDs治疗的患者≤基线3个月与基线后>3个月开始bDMARDs的受试者相比,处于快速改进轨迹比缓慢改进轨迹的几率高3.6倍(95% CI 1.32–10.0;P = 0.013)。第一次风湿病就诊时的短病程作为不用bDMARD治疗的有利轨迹的预测因子接近统计学差异。
结论:在未经治疗的多关节JIA受试者中,在基线评估的3个月内开始 bDMARDs与更快实现非活动性疾病相关。这些结果证明了病程轨迹分析作为确定治疗效果的一种方法。
出处:
Ong MS, Ringold S, Kimura Y, Schanberg LE, Tomlinson GA, Natter MD; CARRA Registry Investigators. Improved Disease Course Associated With Early Initiation of Biologics in Polyarticular Juvenile Idiopathic Arthritis: Trajectory Analysis of a Childhood Arthritis and Rheumatology Research Alliance Consensus Treatment Plans Study. Arthritis Rheumatol. 2021 Oct;73(10):1910-1920. doi: 10.1002/art.41892. Epub 2021 Aug 27. PMID: 34105303.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#生物制剂#
22
#Arthritis#
38
#特发性#
19
#关节炎#
18
#ART#
25