转移性激素敏感型前列腺癌如何治疗?XTANDI(enzalutamide)有望获得欧盟批准
2021-03-27 Allan MedSci原创
制药公司Astellas今天宣布,欧洲药品管理局(EMA)的人用药品委员会(CHMP)对XTANDI(enzalutamide)治疗转移性激素敏感型前列腺癌(mHSPC)的申请持积极意见。
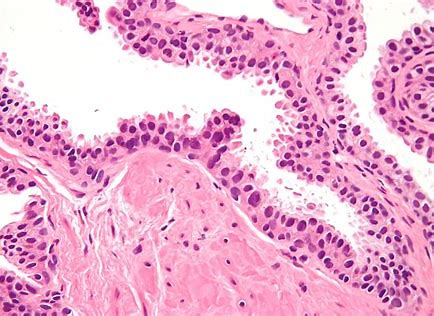
前列腺癌(Prostate cancer)是出自前列腺的恶性肿瘤。大多数前列腺癌生长速度较为缓慢,但仍有些生长相对快速。癌细胞可转移到骨头和淋巴结等部位。前列腺癌早期可能没有症状,晚期可导致排尿困难、尿血、背痛、骨盆疼痛等症状。
制药公司Astellas今天宣布,欧洲药品管理局(EMA)的人用药品委员会(CHMP)对XTANDI(enzalutamide)治疗转移性激素敏感型前列腺癌(mHSPC)的申请持积极意见。XTANDITM(enzalutamide)已经获得批准的适应症为mCSPC。而mHSPC患者预后往往较差,中位生存期约为3-4年,从而强调了对新疗法的需求。
如果获得欧洲药品管理局(EMA)的批准,enzalutamide将是经MEA批准的唯一可用于治疗三种不同类型的晚期前列腺癌-非转移性和转移性去势抵抗性前列腺癌(CRPC)和mHSPC的口服治疗方法。
CHMP这项决定基于关键性III期ARCHES试验的数据。数据表明,与安慰剂联合ADT相比,enzalutamide联合雄激素剥夺疗法(ADT)将mHSPC患者的放射显影或死亡的风险显著降低了61%(P <0.0001)。
Astellas肿瘤高级副总裁Andrew Krivoshik表示:“CHMP的这一积极观点证明了我们致力于满足晚期前列腺癌男性医疗需求的承诺”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Xtandi#
25
转移性激素敏感型前列腺癌
0
#性激素#
36
#转移性#
28
#Enzalutamide#
32
#欧盟批准#
33
我学到了很多东西谢谢老师
51
前列腺癌相关研究,学习了,谢谢梅斯
41