Neurosurgery:血管内栓塞未破裂脑AVM还不如保守治疗好!
2018-05-26 杨中华 脑血管病及重症文献导读
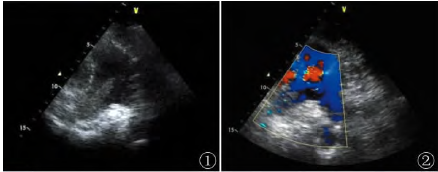
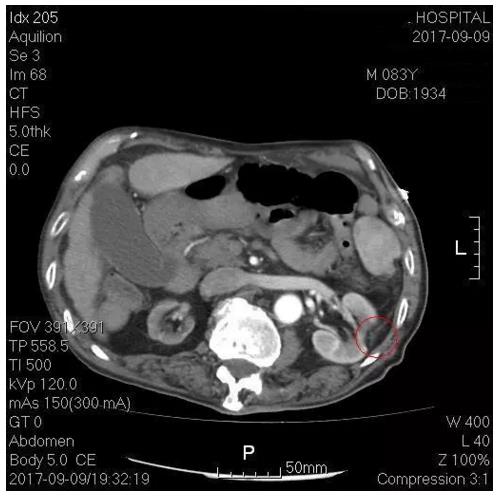
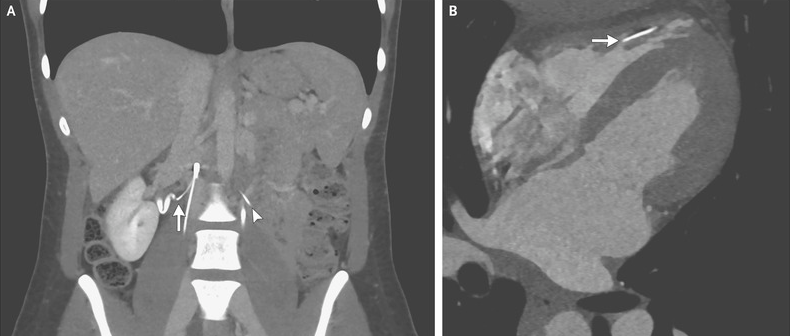
传统上讲,血管内栓塞是显微外科或放射外科治疗脑动静脉畸形(AVM)的辅助手段。然而,随着血管内治疗方法的改进,越来越多的人认为血管内栓塞可以作为治疗脑AVM的方法。但是,对于较小、表浅、栓塞风险较低的AVM,血管内治疗的栓塞率仍然明显低于显微外科手术或放射手术。尽管血管内治疗的病例分析研究发现闭塞率逐渐提高,但是这些研究报道的闭塞率(从2.3%-100%)和死亡率(0%-22.2%)差异很大,提示
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AVM#
46
#surgery#
37
#GER#
26
很有意思的研究
70
#ROS#
36
#保守治疗#
30
学习了.长知识
57