Clin Gastro H: 每日步数与社区性肝硬化患者住院和死亡的高风险相关
2022-07-31 xuyihan MedSci原创
肝硬化是临床常见的慢性进行性肝病,由一种或多种病因长期或反复作用形成的弥漫性肝损害。在我国大多数为肝炎后肝硬化,少部分为酒精性肝硬化和血吸虫性肝硬化。
身体虚弱在终末期肝病 (ESLD) 患者中普遍存在,如今,根据经过验证的虚弱指标评估,近四分之一的ESLD患者符合虚弱标准。肝硬化患者虚弱的高患病率很大程度上与他们的生活方式有关,高达 95% 的白天总时间处于久坐状态。增加体力活动已被证明可以改善肌肉功能和肌肉质量。然而,由于缺乏可及性、安全问题以及运动专业人员治疗 ESLD 患者的专业知识有限,肝硬化患者的运动干预存在滞后。每日步数是心肺健康的衡量标准,可以通过个人活动追踪器 (PAT) 获得。它提供了比自我报告的活动更准确和客观的数据。先前已表明,较高的步数与美国普通成年人群和患有慢性疾病(如慢性阻塞性肺病和心力衰竭)的患者的全因死亡率较低相关。然而,肝硬化患者的步数、虚弱和临床结果之间的关联在很大程度上仍未得到探索。本研究的主要目的是评估每日步数在预测入院率和死亡率方面的效用。
为此,研究人员将所有参与者均进行了肝衰弱指数的评估,以及6分钟步行测试和步态速度测试的衰弱评估。为了监控步数,参与者获得了个人活动跟踪器 (PAT)。还邀请了一个子集使用运动和肝脏 FITness (EL-FIT)。研究了使用PAT第一周的每日步数和虚弱指标作为入院和死亡率的预测因子。

研究结果显示本项研究共纳入116名患者。肝硬化的主要病因是酒精相关(33%)和非酒精性脂肪性肝炎(30%)。80%同时接受PAT+EL-FIT的参与者完成了一周的监测,而仅接受PAT的参与者为 62%(P = .04)。在随访评估期间,55%的患者入院,15%的患者死亡。Kaplan-Meir曲线显示,在最低四分位数(即<1200 步/天)的患者中,再入院率和死亡人数增加。当通过模型调整终末期肝病钠和 EL-FIT 使用时,最低四分位数与住院和死亡均相关(风险比,HR [95% 置信区间],1.90 [1.09–3.30] 和 3.46 [1.23 –9.68])。
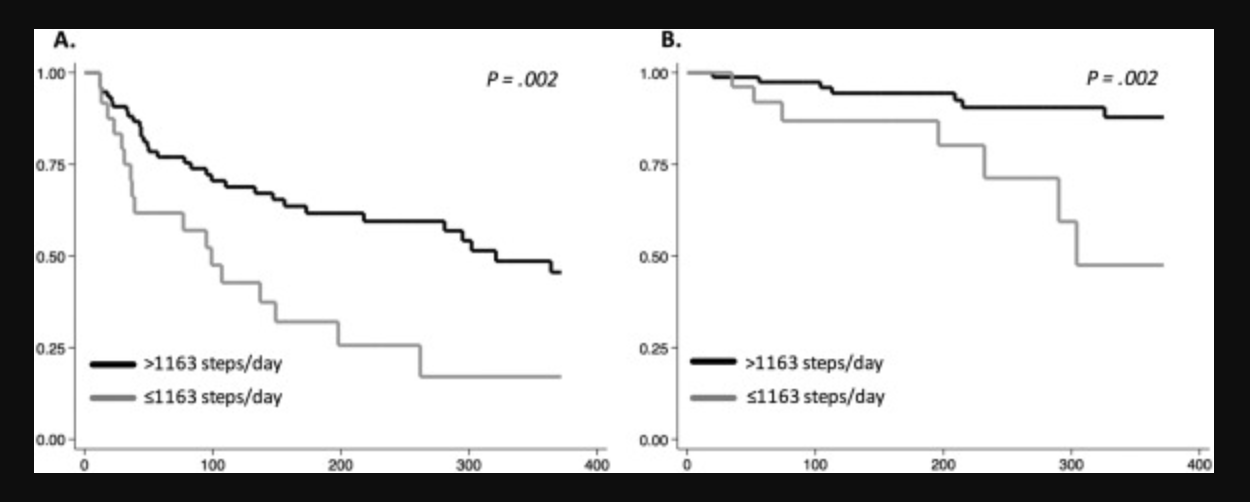
本项研究证实每日步数可以预测肝硬化患者的住院率和死亡率,类似于目前的标准虚弱指标。
原始出处 :
Fei-Pi Lin. et al. Low Daily Step Count Is Associated With a High Risk of Hospital Admission and Death in Community-Dwelling Patients With Cirrhosis. Clinical Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AST#
51
#高风险#
0
#GAS#
41
#社区#
55