J Clin Oncol:依维替尼联合阿扎胞苷治疗新确诊的急性髓系白血病
2020-11-02 星云 MedSci原创
Ivosidenib(依维替尼)是突变型异柠檬酸脱氢酶1(IDH1)的一种口服抑制剂,已获批用于治疗IDH1突变型(mIDH1)急性髓细胞性白血病(AML)。既往研究表明,将阿扎胞苷加入依维替尼可增强
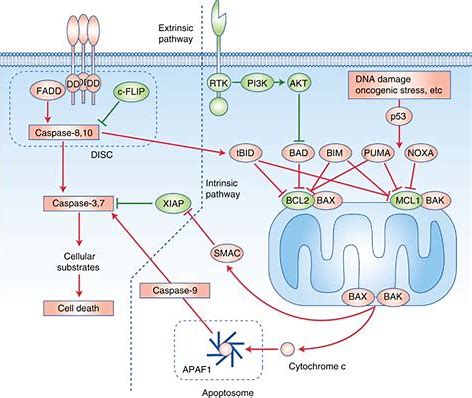
Ivosidenib(依维替尼)是突变型异柠檬酸脱氢酶1(IDH1)的一种口服抑制剂,已获批用于治疗IDH1突变型(mIDH1)急性髓细胞性白血病(AML)。既往研究表明,将阿扎胞苷加入依维替尼可增强mIDH1抑制相关的分化和凋亡。
该研究是一项开放标签、多中心的Ib期试验,旨在评估依维替尼(500 mg,1/日,口服)联合阿扎胞苷(75 mg/m2,28天疗程的前7天用药,皮下注射)用于不适合做强化诱导化疗的新确诊的mIDH1 AML患者的疗效和安全性。
副作用情况
共23位患者接受依维替尼联合阿扎胞苷治疗(中位年龄76岁)。发生于10%以上的患者的治疗相关≥3级不良反应有中性粒细胞减少(22%)、贫血(13%)、血小板减少(13%)和心电图QT间期延长(13%)。令人特别关注的不良反应包括所有级别的IDH分化综合征(17%)、所有级别的心电图QT间期延长(26%)和≥3级白细胞增多症(9%)。

治疗期间的缓解和IDH1突变状态变化
中位治疗持续15.1个月;截止2019年2月19日,10位患者仍在继续治疗。总体缓解率为78.3%(18/23),完全缓解率为60.9%(14/23)。中位随访16个月,缓解患者的中位缓解持续时间未达到。12个月存活率估计为82.0%。14位获得完全缓解的患者中有10位(71.4%)的骨髓单核细胞中的mIDH1得以清除。
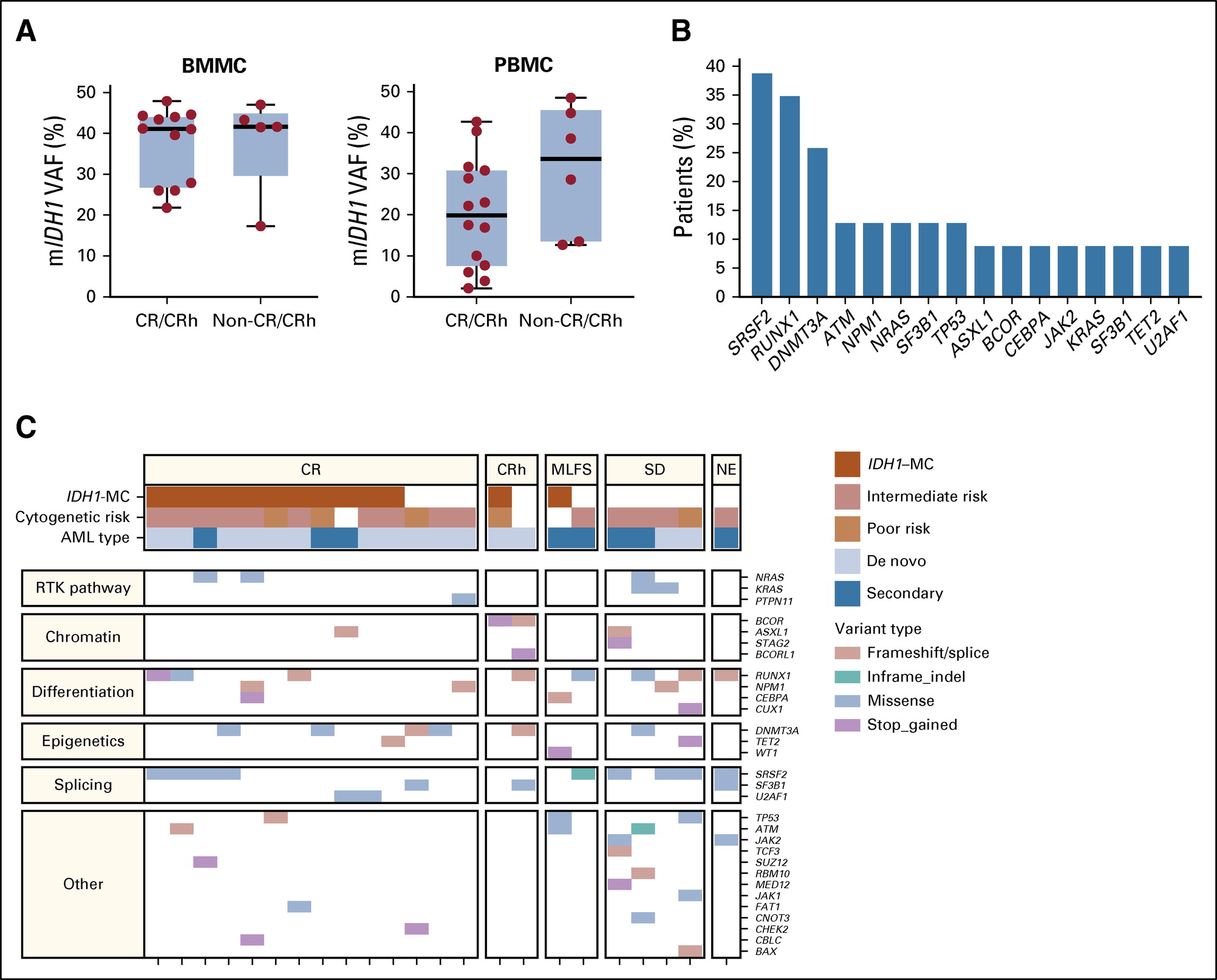
共有突变和临床预后的相关性
总之,依维替尼联合阿扎胞苷的耐受性良好,预期安全性与每种药物的单药疗法一致。缓解彻底且持久,而且大部分完全缓解患者可达到mIDH1突变清除。
原始出处:
Courtney D. DiNardo, et al. Mutant Isocitrate Dehydrogenase 1 Inhibitor Ivosidenib in Combination With Azacitidine for Newly Diagnosed Acute Myeloid Leukemia. Journal of Clinical Oncology. October 29, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#髓系白血病#
28
#Oncol#
27
了解
107
谢谢梅斯分享这么多精彩信息
62
#依维替尼#联合#阿扎胞苷#治疗新确诊的#急性髓系白血病#,总体缓解率为78.3%(18/23),完全缓解率为60.9%(14/23)。这个数据很牛!
0
好文章,学习了!
86
学习了
94
好好学习
92
学习
19
好
25