Breast Cancer Res Treat:局部亚微米颗粒紫杉醇可有效治疗乳腺癌皮肤转移
2022-07-18 MedSci原创 MedSci原创
乳腺癌患者的皮肤转移并不少见,发病率在5%至10%之间。近日,一项1/2期研究评估了无水软膏基质的局部亚微米颗粒紫杉醇(SPP)治疗发生皮肤转移的效果。
乳腺癌患者的皮肤转移并不少见,发病率在5%至10%之间。近日,发表于Breast Cancer Res Treat的一项1/2期研究评估了无水软膏基质的局部亚微米颗粒紫杉醇(SPP)治疗发生皮肤转移的乳腺癌患者的安全性和有效性。
在3+3一期设计中,每天两次将三种浓度的SOR007 SPP之一(0.15%、1.0%或2.0%)涂抹在50平方厘米的患区区域内,持续28天,一旦安全性得到确认,可选择在2a期中以最高剂量再延长28天。通过病变测量和照片分析疗效,以确定总缓解率(ORR)、完全缓解(CR)和第28天或56天的无进展生存期。
结果,研究共纳入23名受试者,其中21人患有乳腺癌皮肤转移(CMOBC)。四名受试者接受SOR007 0.15%的剂量,中位数为28天(范围=17-29),三名接受1.0%的剂量,中位数为28天(范围=6-29),16名接受2.0%的剂量,中位数为55天(范围=6-60)。观察结果显示,所有剂量都有良好的耐受性,19名受试者可进行疗效评估。在所有剂量水平的第28天,16%(95% CI 3.4至39.6%)的受试者达到了ORR,另外63%(95% CI 34.9-96.8%)的受试者病情稳定(SD)。在所有治疗中,28天无进展的患者比例为79%(95CI为54-94%)。
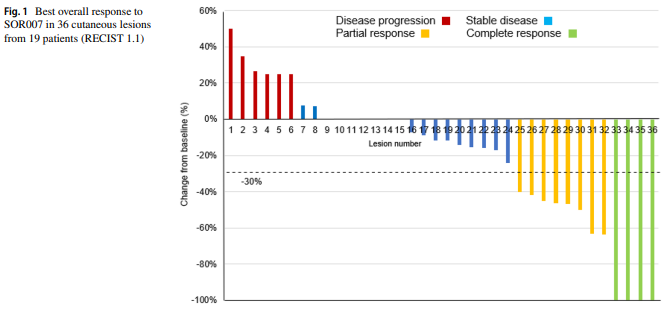
综上所述,该研究结果表明,将SOR007 0.15%、1.0%和2.0%应用于皮肤转移的乳腺癌患者,安全且耐受性良好,病灶疼痛有所减轻,紫杉醇的全身吸收量很小。在研究期间,大多数受试者都观察到病变的稳定。有必要进行随机、安慰剂对照试验来进一步证实这些发现。
原始出处:
Mario E Lacouture, et al., Phase 1/2 study of topical submicron particle paclitaxel for cutaneous metastases of breast cancer. Breast Cancer Res Treat. 2022 Jul;194(1):57-64. doi: 10.1007/s10549-022-06584-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#皮肤转移#
43
#TREAT#
54
#AST#
45
学习
40
#Breast#
57
#局部#
40
#有效治疗#
55