Future Oncol:适合于东亚结直肠癌患者MSI检测位点新研究
2018-07-05 佚名 肿瘤资讯
近日,国际肿瘤期刊《Future Oncology》发表的一篇题为“The clinicopathological features and prognosis of tumor MSI in East Asian colorectal cancer patients using NCI panel”文章,通过对东亚结直肠癌(CRC)患者不同MSI检测位点进行对比,确定出最佳MSI检测Panel,
近日,国际肿瘤期刊《Future Oncology》发表的一篇题为“The clinicopathological features and prognosis of tumor MSI in East Asian colorectal cancer patients using NCI panel”文章,通过对东亚结直肠癌(CRC)患者不同MSI检测位点进行对比,确定出最佳MSI检测Panel,并对东亚结直肠癌MSI发生率,临床病理特征及预后的相关性进行分析总结。该研究由上海长海医院、华中科技大学同济医学院附属协和医院及上海桐树生物科技等3家科研机构共同完成,为MSI(微卫星不稳定性)在结直肠癌患者的诊断、临床病理特征及预后意义等方面提供重要的临床指导意义。
一分钟看全文
本文研究人员采用两种不同检测位点测定MSI,并结合MMR蛋白免疫组化实验和多元变量分析,探究东亚CRC患者MSI的发生状况、临床病理特征及预后的相关性,研究主要得到以下发现:
●东亚CRC患者MSI发生率略低于欧美人群,人群种族及基因多态性的不同,导致微卫星重复系列存在差异。
●单核苷酸+双核苷酸联合Panel敏感性高于单纯单核苷酸Panel,对于东亚裔CRC患者MSI的检测,单核苷酸+双核苷酸联合Panel更适合。
●东亚裔MSI的临床病理特征与欧美人群基本一致,MSI-H好发于二期、近端、右半结肠部位,且分化较差伴有粘液成分的CRC患者。
读完之后,此刻你是否还意犹未尽,想对文章细节进行更深入的了解呢?别急,小编在此为您进行了详细的整理,您想要的都在这里哦!
研究背景
结直肠癌(CRC)是最常见的恶性肿瘤之一,据统计,全球每年约有 120 万名患者被确诊为结直肠癌,而有超过 60 万名患者直接或间接死于结直肠癌。因此,结直肠癌已成为现阶段威胁人类健康的重要疾病之一。近年来,随着分子生物学及相关基因组学的发展,人们发现MSI在CRC的精准诊断和治疗中扮演者极其重要的角色,如对CRC预后进行判断,指导5-氟尿嘧啶、伊立替康等化疗药物的反应,帮助诊断筛选Lynch综合征等,MSI已成为结直肠癌预后和临床辅助治疗过程中一个重要分子标志物。
对于结直肠癌MSI的检测,早在2004年,美国国立癌症研究中心(NCI)颁布了贝塞斯达(Bethesda)标准,该标准在MSI检测位点的选择上规定了两种方式:2个单核苷酸(BAT-25、BAT-26)+3个双核苷酸(D5S346、D2S123、D17S250)联合位点的NCI Panel或者5个单核苷酸(BAT-25、BAT-26、NR21、NR22、NR24)单纯位点的Pentaplex Panel。尽管这两种Panel均能准确的检测MSI,但经比较发现,二者在检测内对照设置、MSI-L精准筛查、MSI判定标准等方面仍存在一定的差异和优劣势。近年来,随着MSI相关研究的不断深入,有研究报道针对东亚裔CRC患者MSI表型检测采用2个单核苷酸+3个双核苷酸的联合Panel可能更为适合,但这种观点需要进一步的研究证实。为此本研究以东亚裔CRC患者为研究对象,采用两种不同的位点对MSI进行检测,并采用MMR蛋白免疫组化对两种方法进行评估,旨在为MSI的检测、临床病理及预后提供一定的理论依据。
研究方法
本研究以245例东亚结直肠癌患者为研究对象,其中直肠癌62例,左半结肠癌107例,右半结肠癌40例,其他类型(包括横结肠癌、横结肠-乙状结肠癌、乙状结肠癌等)36例。
采用PCR和IHC对患者MSI和MMR蛋白进行检测,在PCR检测MSI过程中,位点选择采用NCI Panel 和Pentaplex Panel两种检测方法对患者的MSI进行检测,并用免疫组化实验评估MMR蛋白表达与两种Panel检测MSI间的一致性,同时通过多元变量分析MSI-H与临床病理特征及相关基因突变信息的相关性,以此为CRC临床诊断及预后评价提供更为完善的参考价值。
研究结果
1. MMR蛋白表达与MSI的相关性比较
目前,MMR蛋白的免疫组化分析(IHC)已成为临床上检测MSI的一种常用方法,通过检测MLH1、MSH2、PMS2及 MSH6 4种蛋白表达,当4种蛋白均为阳性时,则判读为MMR-I(MMR蛋白完整),如果其中一个蛋白表达缺失则判读为MMR-D(MMR蛋白缺失)。本研究通过采用IHC对患者4种蛋白检测,发现共有28例患者为MMR-D,这28例患者12例(42.9%)为1个蛋白缺失,16例患者(57.1%)为两个蛋白缺失。
对于MSI表型的检测,我们分别采用NCI Panel和Pentaplex Panel两种方法进行检测。在NCI Panel 检测中我们发现有27例患者(11%)为MSI-H表型,2例患者(0.8%)为MSI-L表型,剩下216例患者(88.2%)为MSS表型;相比对于Pentaplex Panel检测,结果显示23例患者(9.4%)为MSI-H表型,1例患者(0.4%)为MSI-L表型,221例患者(90.2%)为MSS表型。值得注意的是,两种方法均发现BAT-25、BAT-26是所有检测位点中最不稳定的,检测灵敏度均大于75%,如图1。
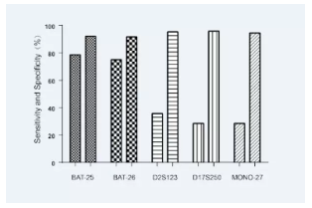
图1 两种方法检测5个MSI标记位点的灵敏度和特异性
2. 不同方法测定MSI状态的一致性比较
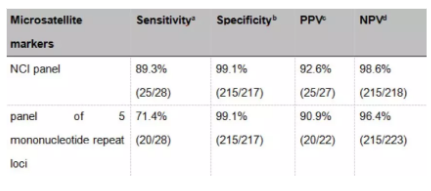
通过比较NCI Panel和Pentaplex Panel两种方法的灵敏度和特异性(见表1),结果发现NCI Panel检测的敏感性高于Pentaplex Panel检测的敏感性,这提示NCI Panel检测可能更适合于东亚裔患者。
表1 微卫星标记在无错配修复蛋白表达检测中的预测值
采用MMR IHC对两种Panel进行评估(见表2,表3),结果发现,与Pentaplex Panel相比,NCI Panel与dMMR的一致性可能更高(Kappa值0.898),这表明NCI Panel检测能更好的反映MMR蛋白表达。
表2 免疫组化检测MMR蛋白表达与NCI Panel检测MSI间的一致性
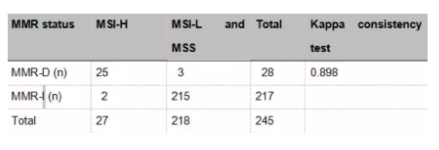
表3 免疫组化检测MMR蛋白表达与五个单核苷酸重复系列检测MSI间的一致性

3. MSI-H与临床病理特征
对于MSI-H与非MSI-H的患者进行比较,发现MSI-H患者与肿瘤分级、右侧肿瘤位置、粘液组织类型相关,与患者年龄、TNM分期、BRAF突变、淋巴结转移不相关。
4. MMR蛋白表达、MSI状态与结直肠癌预后
本研究对245名患者进行为期24个月的随访,结果发现MSI-H患者相比MSS / MSI-L患者有更长的无病生存期(DFS)(图2),同样,MMR蛋白表达缺失(MMR-D)患者较MMR蛋白表达完整(MMR-I)患者表型有更长的无病生存期(DFS)。以上结论表明MMR-D和MSI-H是CRC患者的两个独立预后因素。
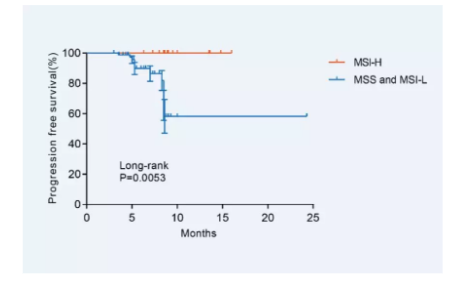
图2 MSI表型与患者DFS间关系
结论
MSI是CRC诊断和治疗领域中一个非常重要的生物标记物,可准确反映CRC病理学特征,同时对CRC的治疗如5-氟尿嘧啶化疗响应也能提供一定的指导,本研究采用两种不同的方法对MSI进行检测比较,并分析MMR蛋白表达、MSI-H与结直肠癌预后间的关系,得到以下结论:
(1)采用NCI Panel对东亚CRC患者MSI进行检测,发现MSI-H约占11%,这一比例较欧美CRC患者(MSI-H约8-20%)略低,这可能与独特的临床病理特征,种族差异及基因多态性相关。
(2)采用NCI Panel 、Pentaplex Panel对MSI进行检测,其中NCI Panel检测分析灵敏度似乎更高,同时与IHC测得的MMR比较,NCI Panel检测的一致性也更好,这可能与两种方法的内对照,cut-off值及MSI发生核苷酸位点相关。
(3)本研究再次证实MSI对CRC患者的预后有一定的指导意义,尤其是MSI-H患者,其无病生存期(DFS)较MSS/MSI-L患者更长,因此MSI-H是CRC治疗预后的一个有效的标志物。
原始出处:
Jianmin Zheng, et al. The clinicopathological features and prognosis of tumor MSI in East Asian colorectal cancer patients using NCI panel. Future Oncology. Jan 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Oncol#
33
结直肠癌靶向药物治疗.
60
适合于东亚结直肠癌靶向药物治疗.
68
学习
70
#结直肠#
33
#MSI#
22
学习
68
学习
60