我就看看我不吃?NO!Cell子刊:仅看一眼食物,就能引发脑内炎症因子分泌
2022-07-11 四五七 MedSci原创
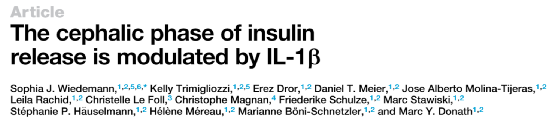
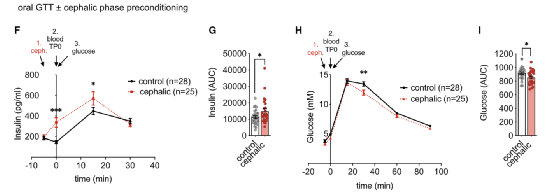
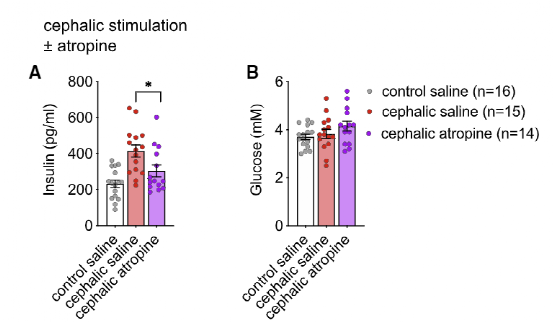
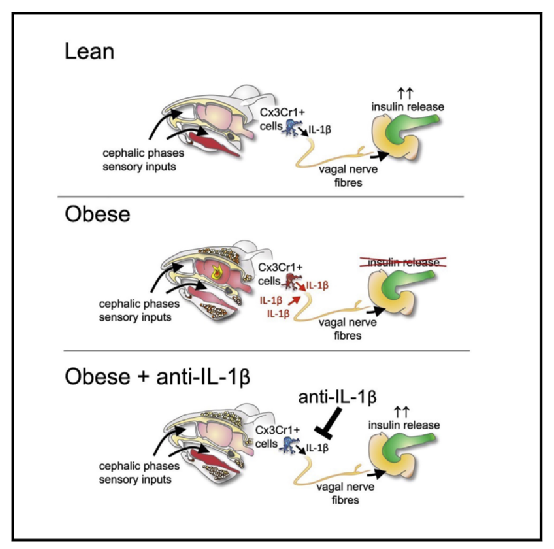
Cell Metabolism:食物刺激引起大脑炎症因子短暂增加,进而激活支配胰腺的副交感神经,在食物还未引起血糖变化前,就促使胰岛β细胞提前释放胰岛素,对降低餐后血糖、维持血糖稳态起着重要作用。

参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
47
#分泌#
58
#CEL#
35
#食物#
44
签到学习
78
学习了
71