Stroke:颈动脉内膜切除术治疗症状性颈动脉狭窄不同分流模式的结局差异
2022-03-27 网络 网络
常规和选择性分流的CEA总体结果相似。在缺血性卒中后<2天进行的CEA,常规分流的术后卒中率较低。
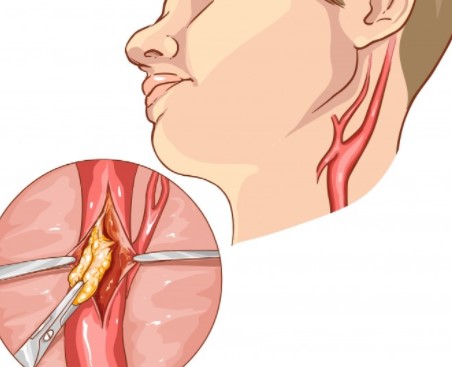
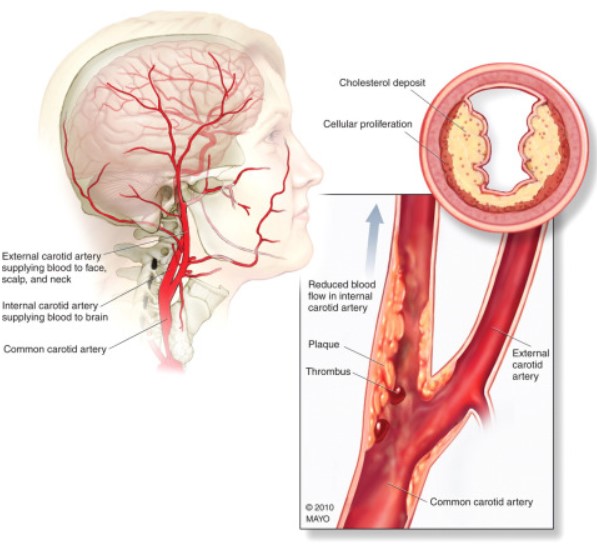
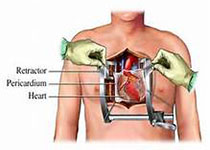
动脉内膜切除手术(CEA)是一种通过纠正总颈动脉或内颈动脉狭窄, 以达到改善大脑供血, 并试图降低中风风险的外科手术。内膜切除手术是指去除附(位)于动脉内膜上的硬化斑快状病变物质, 而这些硬化物质往往是导致动脉内腔狭窄和阻塞的原因。
为了评估外科医生的分流做法和分流的使用对近期有症状患者的颈动脉内膜切除术(CEA)的早期结果的影响,来自mayo诊所脑血管外科的专家开展了相关研究,结果发表在Stroke杂志上。
研究人员在多中心国家前瞻性数据库的基础上进行了一项回顾性观察研究。血管质量倡议数据库(2010-2019)查询了同侧中风或短暂性脑缺血发作后14天内进行的CEA。如果外科医生在大于95%的CEA中进行分流,则被视为常规分流者,否则被列为选择性分流者。根据指标事件的类型(短暂性脑缺血发作与中风)和CEA的时间(≤2天与>2天),对常规分流者和选择性分流者的院内中风率和死亡率进行了比较。
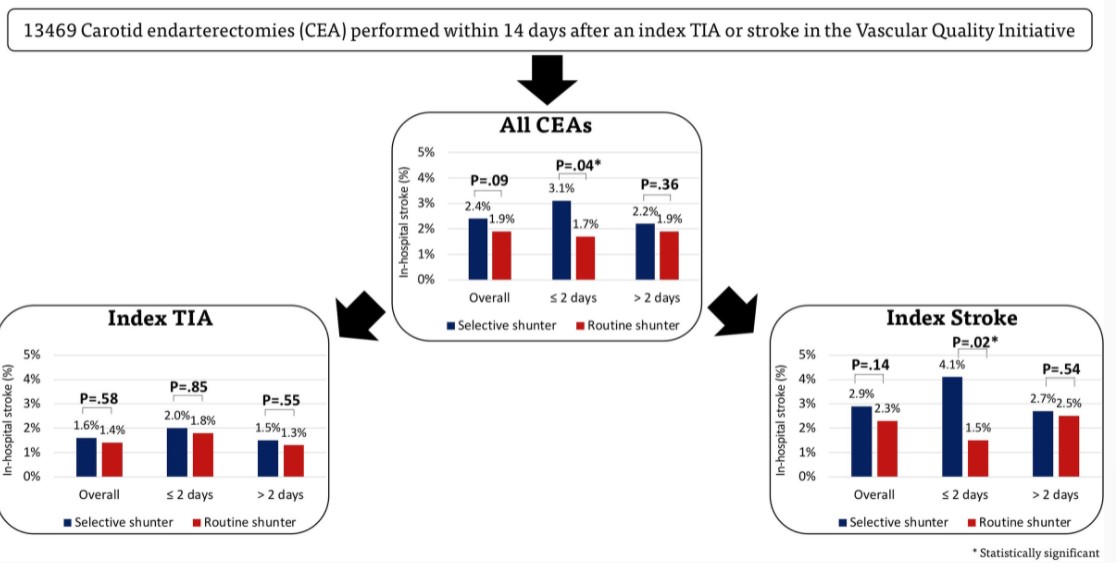
13469例CEA是在短暂性脑缺血发作(43%)或中风(57%)后进行的,3186例(24%)由常规分流进行,10283例(76%)由选择性分流进行。比较常规和选择性分流,院内中风(1.9% vs 2.4%;P=0.09)和死亡(0.4% vs 0.5%;P=0.73)率相似。
在缺血性卒中后<2天进行CEA的常规分流,卒中率较低(1.5% vs 4.2%;P=0.02)。在选择性分流中,使用分流的情况下发生较高的中风率(2.9% vs 2.3%;P<0.01),主要是由于出现中风发作(3.5% vs 2.4%;P<0.01),而不是TIA(1.8%vs1.5%;P=0.57)。
此外,选择性分流术者有7.8%的病例采用清醒麻醉,常规分流术者有0.8%的病例采用清醒麻醉,但对围手术期的卒中率没有影响(1.8%vs2.3%;P=0.349)。
在这个大型国家队列中,常规和选择性分流的CEA总体结果相似。在缺血性卒中后<2天进行的CEA,常规分流的术后卒中率较低。在选择性分流中,术中指示分流决定了中风率的增加,可能是由于术中灌注不足。这些数据可以指导对有症状的患者进行CEA的时机和分流意向的决定。
参考文献:
Impact of Shunting Practice Patterns During Carotid Endarterectomy for Symptomatic Carotid Stenosis.Stroke. 2022;0:STROKEAHA.121.037657. https://doi.org/10.1161/STROKEAHA.121.037657.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#症状性颈动脉狭窄#
42
#颈动脉#
48
#内膜#
39
#切除术#
34
学习
49
#动脉狭窄#
31