Liver Cancer:TACTICS研究表明在TACE基础性加用索拉非尼可改善不可切除肝细胞癌(HCC)患者的PFS,但不能改善患者的OS
2022-02-21 yd2015 MedSci原创
TACTICS研究表明,在TACE基础性加用索拉非尼可改善不可切除肝细胞癌(HCC)患者的PFS,但不能改善患者的OS。
很多临床试验比较了经动脉化疗栓塞(TACE)联合分子靶向药物对比单独TACE治疗不可切除肝细胞癌的疗效和安全性,结果显示在无进展生存期(PFS)或总生存期(OS)方面没有临床益处。近期,Liver Cancer杂志上报道了来自日本的临床研究TACTICS(NCT01217034)的最终OS分析结果,该研究先前表明,TACE联合索拉非尼在不可切除的肝细胞癌(HCC)患者的PFS有显著改善。
不能切除的HCC患者被随机分为TACE +索拉非尼组(N=80)和TACE单独组(N=76)。TRAE特异性PFS被定义为从随机分组到进展性疾病(PD)或任何原因导致死亡的时间,PD被定义为无法治疗(UnTACEable)的进展,包括根据 RECICL标准评估的肝内肿瘤进展(比基线增加>25%)、肝外扩散、血管侵犯或TACE后肝功能短暂恶化至Child-Pugh C等原因。
2011年2月-2016年3月,共筛查了197名患者;其中156例符合纳入标准。在156例入组患者中,60例(38%)患者为BCLC -A期;多数患者为单发大肿瘤(>5cm)。18例(12%)患者根据ECOG=1并且无EHS或MVI将肿瘤归类为BCLC - C期。其余78例(50%)患者为BCLC-B期。

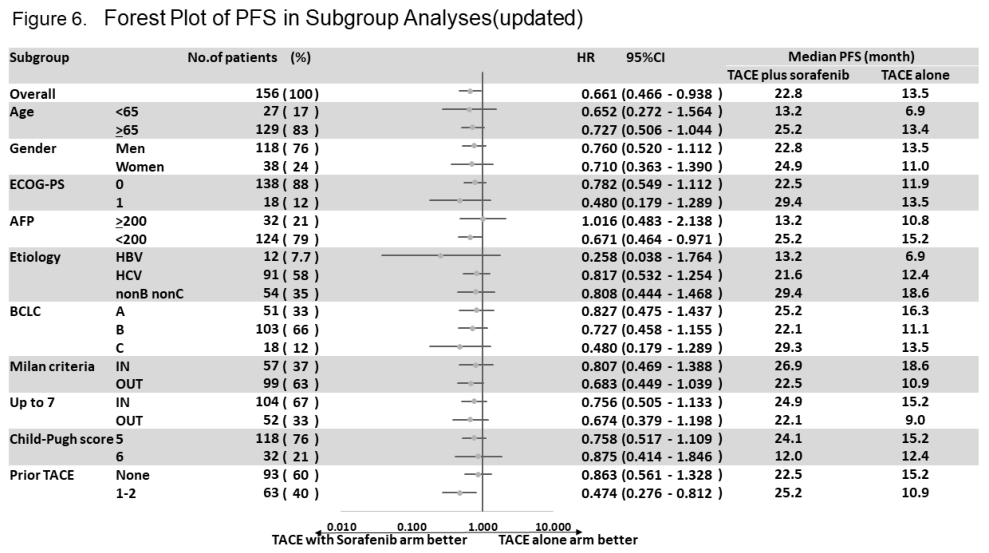
既往有研究报道了主要研究终点TRAE特异性PFS结果,结果显示TACE+索拉非尼治疗较单独TACE治疗显著延长TACE-特异性PFS (25.2 vs. 13.5个月; HR=0.59; 95% CI, 0.41–0.87; P=0.006)。
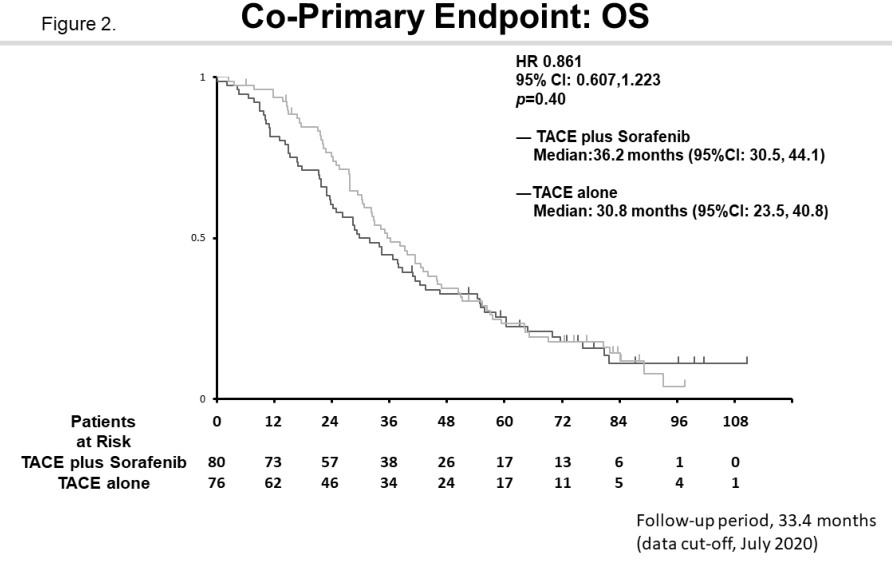
基于PFS的阳性结果,研究进行了OS分析。TACE +索拉非尼组的中位OS为36.2个月(95% CI, 30.5-44.1),而TACE单药组的中位OS为30.8个月(95% CI, 23.5-40.8)。因此,TACE联合索拉非尼并没有比TACE单药治疗提供更大的生存益处(HR= 0.861;95%CI: 0·607-1·223;P = 0·40)。
亚组分析显示,在考虑大多数因素时,TACE +索拉非尼组的OS优于TACE单药治疗组。
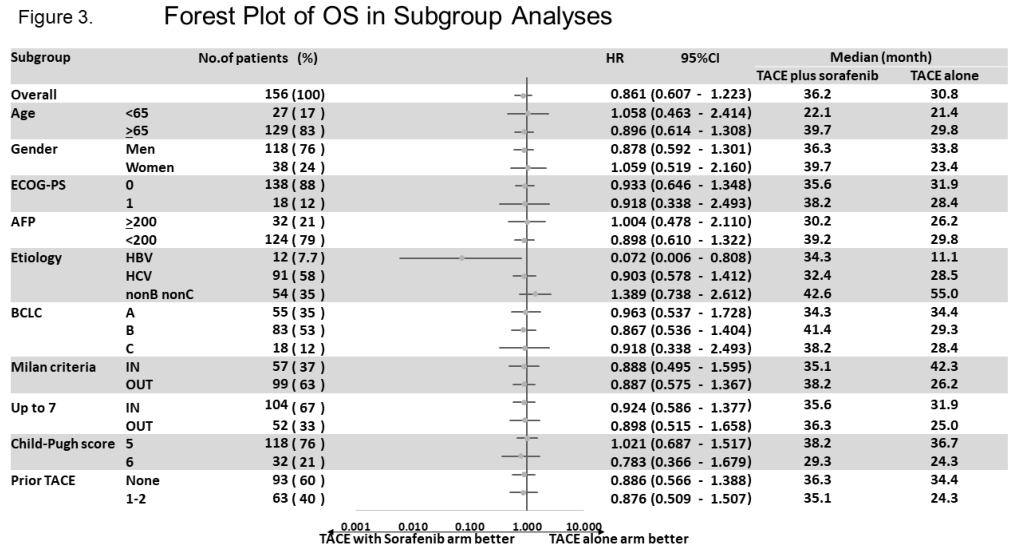
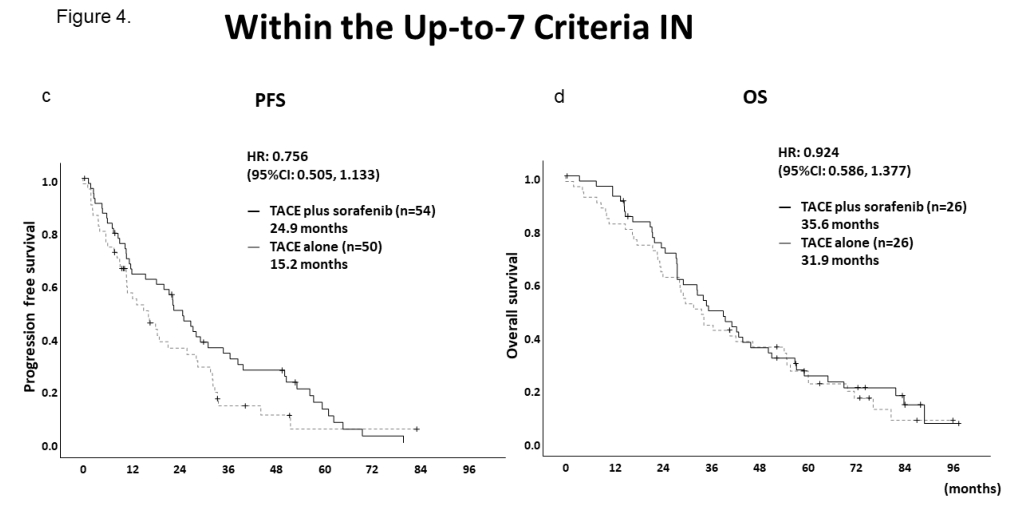
预先设置的分析显示,在不符合 up-to-seven标准的患者中,TACE单独组的中位OS为25.0个月,TACE +索拉非尼组的中位OS为36.3个月,数值上改善了11.3个月。在符合up-to-seven标准的患者中,TACE单独组和TACE +索拉非尼组的中位OS分别为31.9个月和33.5个月,数值上改善了3.7个月。在不符合 up-to-seven标准的患者中,TACE单药治疗组中位TACE特异性PFS为9.0个月,而TACE +索拉非尼组延长至22.1个月(HR=0.674; 95% CI, 0.379–1.198);在符合up-to-seven标准的患者中,TACE单药治疗组中位TACE特异性PFS为15.2个月,而TACE +索拉非尼组延长至24.9 个月(HR=0.756; 95% CI, 0·505–1.133)。

更新的TACE特异性PFS显示,TACE联合索拉非尼组的中位TACE特异性PFS为22.8个月(95% CI, 18.4-27.5),而TACE单药治疗组为13.5个月(95% CI, 9.2-20.6)(HR=0.661;95% ci, 0.466 0.938;P = 0.02),这些数据与初步分析结果一致。

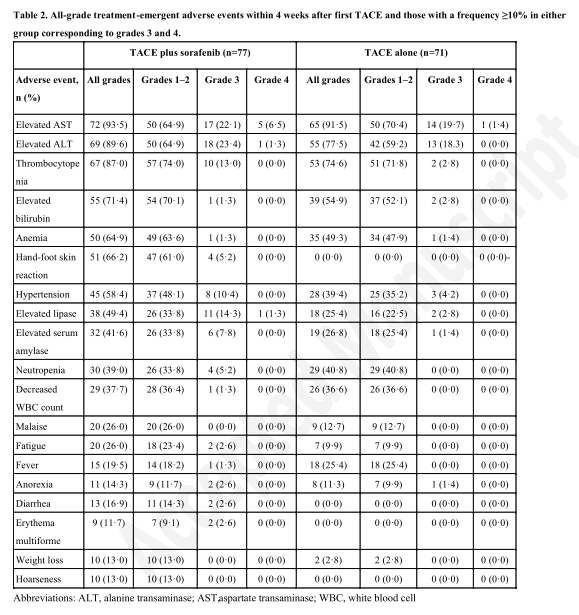
与单纯TACE组相比,TACE+索拉非尼组患者出现了更多的不良反应(AE),包括手足皮肤反应(66·2% vs 0·0%)、高血压(58·4% vs 39·4%)、脂肪酶升高(49·4% vs 25·4%)、疲劳(26·0% vs 9·9%)、腹泻(16·9% vs 0·0%)、多形性红斑(11·7% vs 0·0%)、体重减轻(13.0% vs. 2.8%),声音嘶哑(11.0% vs. 0·0%)。
综上,TACTICS研究表明,在TACE基础性加用索拉非尼可改善不可切除肝细胞癌(HCC)患者的PFS,但不能改善患者的OS。
原始出处:
Kudo M, Ueshima K, Ikeda M,et al. Final Results of TACTICS: A Randomized, Prospective Trial Comparing Transarterial Chemoembolization Plus Sorafenib to Transarterial Chemoembolization Alone in Patients with Unresectable Hepatocellular Carcinoma. Liver Cancer , DOI: 10.1159/000522547. Published online: February 10, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TAC#
39
#ACE#
0
#肝细胞#
39
#细胞癌#
36
学习了
53
受益匪浅
52
#HCC#
43
#PFS#
49