Lancet Oncol:满足 vs 不满足USPSTF筛查标准的肺癌患者,5年生存率相似
2019-06-30 Lisa 肿瘤资讯
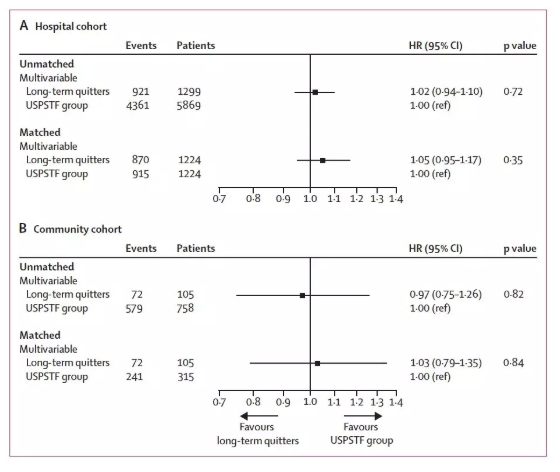
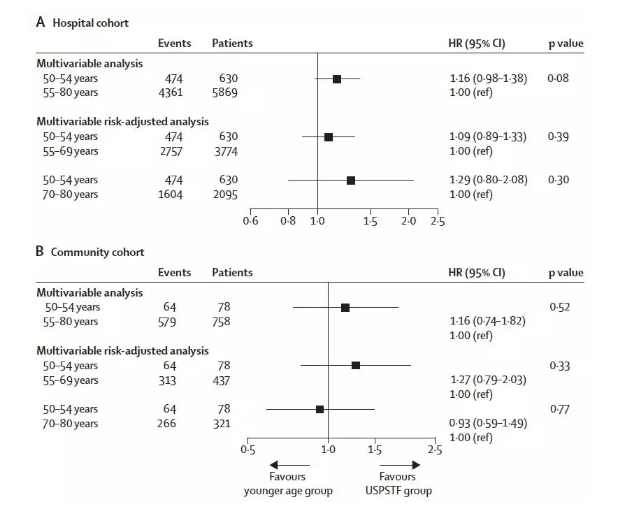
美国预防服务工作小组(USPSTF)推荐对年龄55-80岁,吸烟史达到30包年及以上或戒烟时间少于15年的人群进行肺癌筛查。然而,临床上很多肺癌患者并不符合这一筛查标准,如年轻肺癌患者和长期戒烟者。近期Lancet Oncology杂志发布的一项研究对满足 vs 不满足USPSTF筛查标准的肺癌患者进行生存对比。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
35
#Lancet#
22
#肺癌患者#
26
#生存率#
30
#USPSTF#
33
mark
66
学习学习学习
69
谢谢梅斯分享这么多精彩信息
41