Innate Immun:MMP9在LPS诱导的炎症中起保护作用,可为根尖周炎的预防和治疗提供了新的方法
2020-10-07 MedSci原创 MedSci原创
基质金属蛋白酶(MMP)家族广泛参与了炎症过程中牙髓和根尖组织的破坏。MMP9与口腔炎症密切相关。尽管如此,MMP9在口腔炎症过程中的具体功能及其机制尚不十分清楚。
基质金属蛋白酶(MMP)家族广泛参与了炎症过程中牙髓和根尖组织的破坏。MMP9与口腔炎症密切相关。尽管如此,MMP9在口腔炎症过程中的具体功能及其机制尚不十分清楚。
我们之前的研究发现,在实验诱导的根尖周炎中,MMP9基因敲除小鼠与野生型小鼠相比,炎症更为严重。此外,与野生型小鼠相比,MMP9基因敲除小鼠牙槽骨破坏的病理现象更加明显。因此,我们提出MMP9具有 "抗炎"特性。
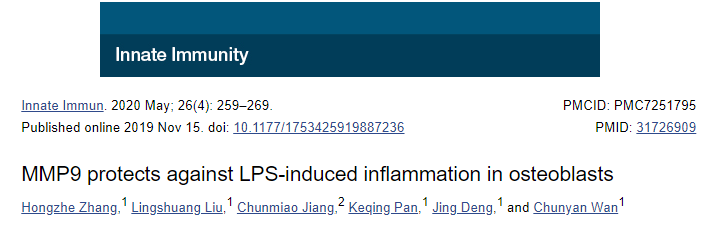
本研究旨在探究MMP9对炎症反应以及对骨形成和骨破坏的影响。qRT-PCR和Western blot显示,MMP9在LPS刺激的MC3T3-E1细胞中减少了IL-1β、TNF-α、RANK、RANKL、TLR2和TLR4的产生。同时,在LPS刺激的细胞中,OPG和OCN的表达量因MMP9而增加。
综上所述,该研究结果表明,MMP9在LPS诱导的炎症中起保护作用,从而为根尖周炎的预防和治疗提供了新的线索。
原始出处:
Hongzhe Zhang, Lingshuang Liu, et al., MMP9 protects against LPS-induced inflammation in osteoblasts. Innate Immun. 2020 May;26(4):259-269. doi: 10.1177/1753425919887236.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
39
#MMP9#
46
#根尖周炎#
0
#LPS#
29
#保护作用#
38