P2X3受体拮抗剂 eliapixant对难治性慢性咳嗽的疗效和安全性
2021-11-20 小文子 MedSci原创
选择性P2X3拮抗剂似乎是治疗难治性慢性咳嗽的一种新方法。
持续存在的慢性咳嗽为难治性慢性咳嗽(RCC),对患者的生理和心理带来巨大影响。发表在Eur Respir J杂志的2a期双盲随机对照研究评估了选择性P2X3受体拮抗剂eliapixant(BAY 1817080)对难治性慢性咳嗽患者的安全性、耐受性和疗效。

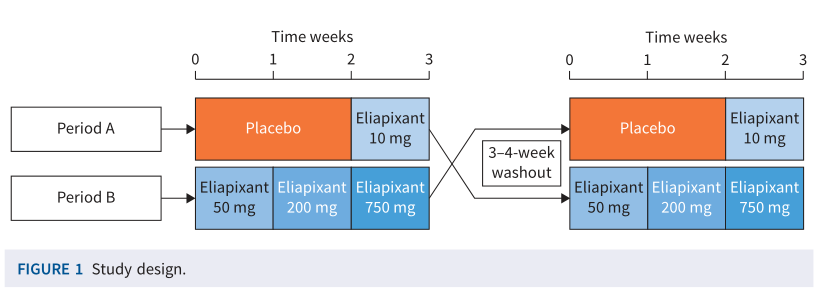
研究纳入18岁以上,体重指数18~35kg/m2,诊断慢性咳嗽1年以上的患者。包括2个治疗阶段,A阶段,患者接受安慰剂治疗2周,然后eliapixant 10mg治疗持续1周。B阶段,患者接受50、200和750mg的eliapixant,每个剂量水平持续1周。患者按1:1的比例随机分为A-B阶段(n=20)或B-A阶段(n=20),中间3~4周洗脱期。基线和每个治疗周的最后一天(第6、13和20天)随访患者。
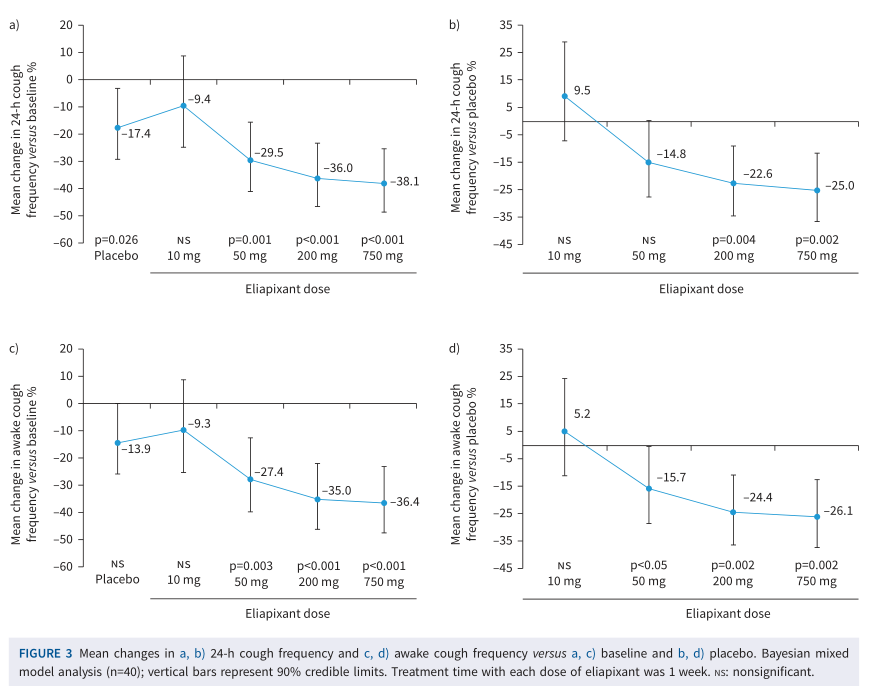
主要疗效终点是24小时期间每小时咳嗽频率的变化。次要疗效终点为患者咳嗽严重程度和咳嗽相关生活质量。主要安全终点是不良事件的发生频率和严重程度。
共37例患者完成了随机治疗。安慰剂组咳嗽频率(24h内测量)相对于基线平均降低17.4%,eliapixant组相对于基线平均降低9.4%~38.1%。eliapixant≥50 mg剂量能够降低咳嗽频率(相比于基线,750 mg剂量降低25%(90%CI, 11.5%~36.5%); p = 0.002)。50 mg剂量同样显著降低咳嗽严重程度。事后分析显示,与安慰剂相比,750 mg剂量组24h内咳嗽频率和清醒咳嗽频率分别降低30.6%和32.1%。使用eliapixant后咳嗽严重程度呈剂量依赖性降低。
65%安慰剂组和41%~49%的eliapixant组患者出现不良反应,大部分为轻度或中度。与味觉相关不良事件的累积发生率在安慰剂组为3%,而eliapixant组为5-21%,均为轻度。
结果显示选择性P2X3拮抗剂eliapixant可显著降低咳嗽频率和严重程度,证实是难治性慢性咳嗽的可行治疗途径,同时治疗剂量下味觉相关副作用较低,表明选择性P2X3拮抗剂似乎是治疗难治性慢性咳嗽的一种新方法。
原文出处:
Morice A, Smith JA, McGarvey L,et al. Eliapixant (BAY 1817080), a P2X3 receptor antagonist, in refractory chronic cough: a randomised, placebo-controlled, crossover phase 2a study.Eur Respir J,2021;DOI: 10.1183/13993003.04240-2020.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#疗效和安全性#
43
指南
45
学习了
48
#拮抗剂#
41
#难治性#
34