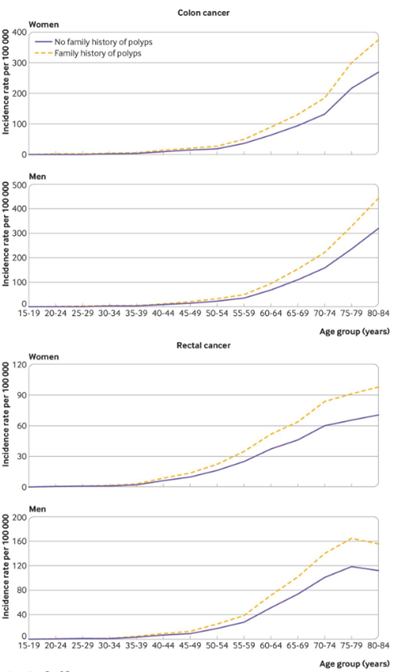
JNCCN:质子泵抑制剂(PPI)可能降低结直肠癌患者的生存
2021-05-11 yd2015 MedSci原创
质子泵抑制剂(PPI)是临床上常用的药物。非癌人群观察性研究中发现,长期服用PPI可出现严重的不良后果,比如增加全因死亡率,心血管疾病,肾脏疾病,低镁血症以及肿瘤等。体内实验发现PPI似乎可有增强某些
质子泵抑制剂(PPI)是临床上常用的药物。非癌人群观察性研究中发现,长期服用PPI可出现严重的不良后果,比如增加全因死亡率,心血管疾病,肾脏疾病,低镁血症以及肿瘤等。体内实验发现PPI似乎可有增强某些抗肿瘤药物的活性。但是,其中的机制不明确。也有观察性和回顾性研究发现,PPI可以降低卡培他滨的疗效,药代动力学以及体内实验也未能解析两者的关系。

因此,来自澳大利亚的研究团队,在Journal of The National Comprehensive Cancer Network (JNCCN) 杂志发表了一项研究数据,评估PPI与氟尿嘧啶治疗为基础的晚期结直肠癌的生存关系。
该研究主要为随机对照研究的二次分析,纳入了6项研究,共5594例患者,其中902例患者使用PPI(使用PPI定义为:自临床实验开始服用任何PPI至少7天)。主要研究总生存(OS),无进展生存(PFS),以及亚组分析,如卡培他滨或5-氟尿嘧啶等。使用随机效应模型计算HR和95%CI。
研究数据显示,PPI 使用跟结直肠癌患者较差的OS相关 (pooled HR, 1.20; 95% CI, 1.03–1.40; P=0.02; I 2 = 69%);
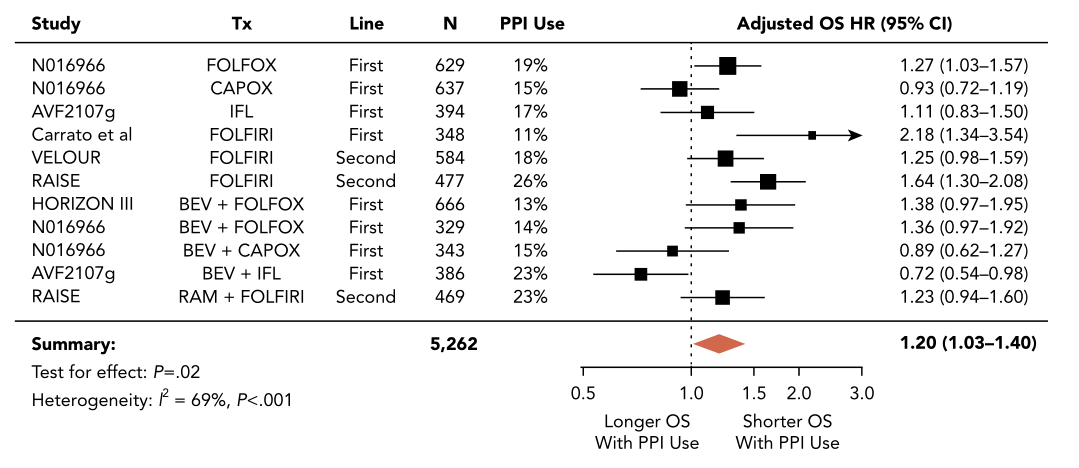
OS分析
同样, PPI 使用跟结直肠癌患者较差的PFS相关 (overall pooledHR, 1.20; 95% CI, 1.05–1.37; P=0.009; I 2 = 65%) 。
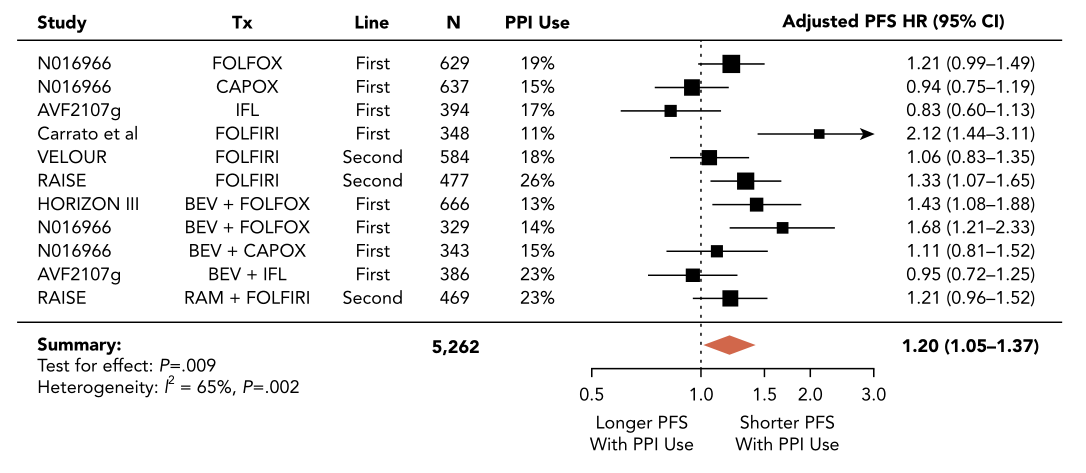
PFS分析
而亚组分析发现PPI的使用在各治疗亚组中的生存关系跟与总体人群中相似。
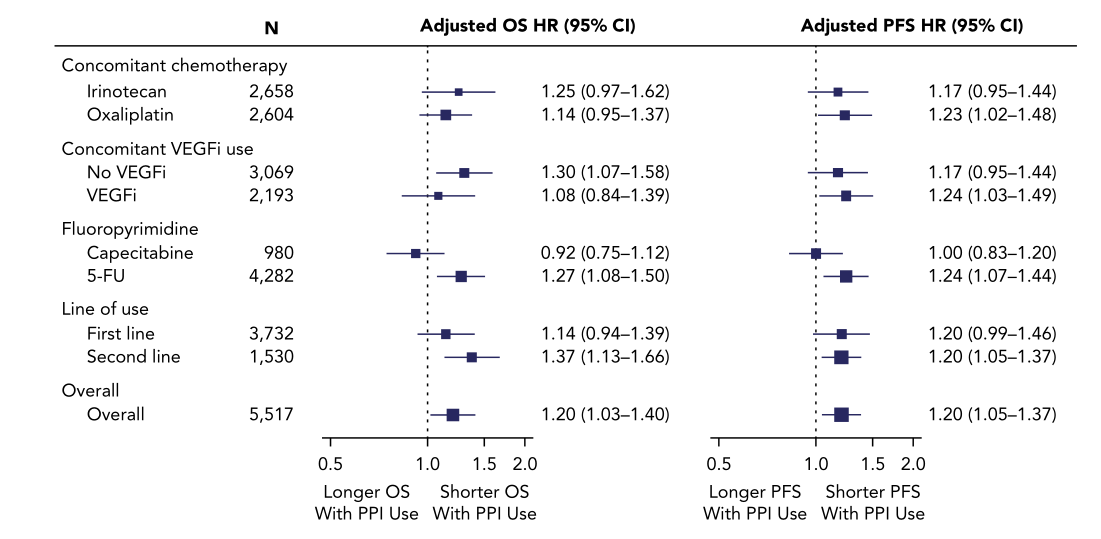
亚组分析
综上,PPI的使用跟氟尿嘧啶为基础治疗的晚期结直肠癌患者较差预后有关。当然,这个需要更进一步的研究。但是也同时提醒我们临床医生,对于这部分患者需要谨慎使用PPI。
原始出处:
Ganessan Kichenadasse, MBBS, FRACP, John O. Miners, et al. Proton Pump Inhibitors and Survival in Patients With Colorectal Cancer Receiving Fluoropyrimidine-Based Chemotherapy. JNCCN. Online Publication Date: 05 May 2021. DOI: https://doi.org/10.6004/jnccn.2020.7670.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抑制剂#
45
#质子泵#
40
跟踪学习
60
#NCCN#
35
#结直肠#
40