AJOG:人类的分娩机制至今是个谜?sFLT1、PlGF水平是否能成为研究突破口?
2021-11-05 MedSci原创 MedSci原创
进行性胎盘功能不全可能是一种生理现象,随着接近和足月孕龄的增加而发生,并促进分娩的开始。
尽管进行了几十年的研究,但关于人类分娩开始的机制尚不清楚。在啮齿动物和一些反刍动物中,妊娠是由黄体中的孕酮维持的,分娩是由黄体溶解开始的。在绵羊中,胎儿下丘脑-垂体-肾上腺(HPA)轴的激活导致胎儿血液中的皮质醇增加,从而诱导胎盘中17-α-羟化酶的表达,这种酶将孕酮转化为雌激素,由此导致孕酮的下降和母体血清中雌二醇的升高,从而引发分娩。

相比之下,在人类和非人灵长类动物中,孕酮或雌激素在分娩前的母体循环水平没有显著变化。本研究旨在验证妊娠晚期胎儿生长减慢或母体血清胎盘缺氧标志物水平升高与早产的关系。研究者观察了2208名初产妇女,进行了连续盲法超声检查和可溶性fms样酪氨酸激酶-1和胎盘生长因子的免疫分析。数据采用logistic回归和Cox回归进行分析。
试验验证了36周胎龄时的胎儿大小与足月分娩时间无关。然而,20周胎龄和36周胎龄之间的胎儿生长与37至38周妊娠时自然分娩的概率呈负相关。在妊娠39至40周时这种相关性较弱,在妊娠41周时没有相关性。对于估计的胎儿体重增长速度,观察到了非常相似的关联。可溶性fms样酪氨酸激酶-1e-胎盘生长因子比率与妊娠37-38周自然分娩的概率呈正相关,这种相关性在妊娠39至40周时较弱,而在妊娠41周时没有相关性。
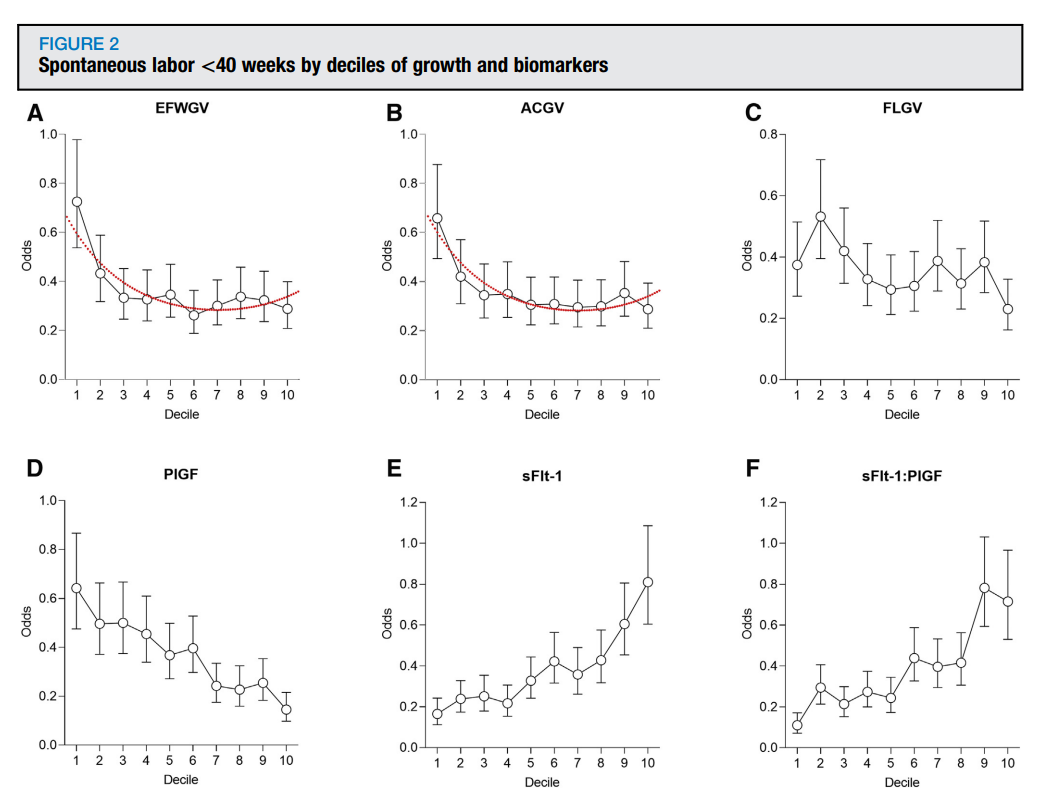
自然分娩小于40周时生长和生物标志物变化水平
总的来说,胎儿生长减慢和胎盘功能不全的生物标志物与早产自然足月分娩的可能性增加有关。研究推测,进行性胎盘功能不全可能是一种生理现象,随着接近和足月孕龄的增加而发生,并促进分娩的开始。
参考文献:Ulla Sovio, Francesca Gaccioli, Emma Cook, D. Stephen Charnock-Jones, Gordon C.S. Smith,
Slowing of fetal growth and elevated maternal serum sFLT1:PlGF are associated with early term spontaneous labor, American Journal of Obstetrics and Gynecology, Volume 225, Issue 5, 2021, Pages 520.e1-520.e10, ISSN 0002-9378, https://doi.org/10.1016/j.ajog.2021.04.232.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#sFLT1#
53
#研究突破#
43
需要进一步研究
53
#分娩#
45
谢谢分享
74