European Radiology:电子密度双能CT对颈椎间盘突出的诊断价值
2022-06-07 shaosai MedSci原创
电子密度(ED)图像是通过使用扫描仪特定的校准曲线转换CT图像上每个像素的HU值来计算应用的辐射剂量。
众所周知,颈椎平扫CT是评估骨折或骨质增生等骨质病变的主要方式。然而,由于其软组织对比度比MRI低,这种技术在显示软组织病变尤其颈椎间盘突出症方面的能力有限。最近许多研究使用先进的CT技术来识别椎间盘突出症。Booz等学者证明,与标准CT(SC)相比,虚拟无钙(VNCa)重建的双能量CT(DECT)对腰椎间盘突出症的诊断准确性可提高>90%。然而,由于椎间盘较小,脑脊液面积较小而脊髓较大,颈椎的椎间盘突出症更难发现。
电子密度(ED)图像是通过使用扫描仪特定的校准曲线转换CT图像上每个像素的HU值来计算应用的辐射剂量。目前,单源双层DECT作为一种无需校准的方法,可以在无需转换为HU的前提下提供更准确的ED maps。它可以通过测量两种不同能量的衰减来区分康普顿散射和光电效应衰减来进行ED成像。尽管ED maps在放射肿瘤学中被广泛用于计算辐射剂量,但这种技术在放射诊断学中还没有被广泛使用。
近日,发表在European Radiology杂志的一项研究以MRI为参考标准,评估了DECT与ED重建在检测颈椎间盘突出症的诊断性能和诊断信心,并与SC和VNCa图像进行了比较。
本项研究招募了64名患者(C2/3至C7/T1的336个椎间盘;平均年龄55岁;17名女性和47名男性),每位患者均在2018年1月至2020年6月期间的2周内接受了DECT与光谱重建和3-T MRI检查。四位放射学家独立评估了随机SC、VNCa和ED图像的第一组图像,以检测颈椎间盘突出症。8周后,读者重新评估第二和最后一组图像,间隔时间为8周。由另外两个有经验的医生进行MRI评估作为参考标准。用广义估计方程来评估每组图像之间的诊断性能。
在MRI上共发现233个颈椎间盘突出症。对于检测颈椎间盘突出症,电子密度图像显示出更高的敏感性(94% [219/233; 95% CI, 90-97] vs. 76% [177/233; 70-81] vs. 69% [160/233; 62-76])。(p < 0.001),特异性与SC和VNCa图像相似(90% [93/103; 83-95] vs. 89% [92/103; 82-96] vs. 90% [93/103; 83-95]) (p > 0.05)。对于所有图像集,四位读者之间计算的颈椎间盘突出症的读者间一致性是中等的(ED的κ = 0.558,SC的κ = 0.422,VNCa的κ = 0.449)。
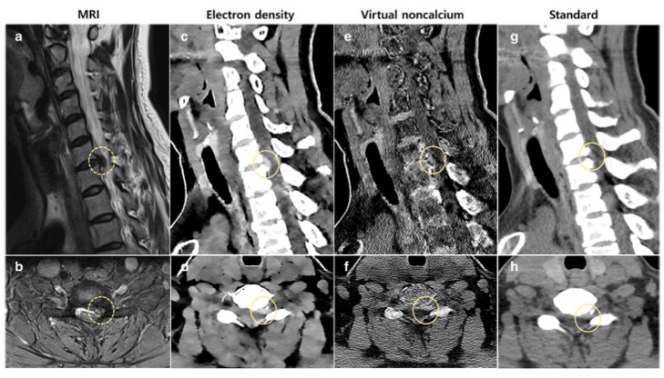
图 48 岁女性,左上肢放射痛。 a、b T2 加权矢状位图像(a)和 T2 加权脂肪抑制轴位图像(b)显示左侧关节下和椎间孔区域的椎间盘突出。 c–h,与虚拟非钙图像(e,f)和标准图像(g,h)相比,电子密度图像(c,d)更清楚地显示椎间盘突出(圆圈)
本研究表明,基于单能量双层DECT的ED图像明显提高了颈椎间盘突出症的检测率,并显示出更高的诊断可信度,甚至在C7/T1层面上也是如此。因此,ED图像有助于诊断仅进行CT扫描患者的颈椎间盘突出症。
原文出处:
Euddeum Shim,Baek Hyun Kim,Woo Young Kang,et al.Diagnostic performance of electron-density dual-energy CT in detection of cervical disc herniation in comparison with standard gray-scale CT and virtual non-calcium images.DOI:10.1007/s00330-021-08374-y.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
54
#双能CT#
40
#椎间盘突出#
49
#诊断价值#
39
学习了
45
学习了,谢谢分享
54