Cancer Discovery: 破坏细胞pH平衡,阻断胰腺癌生长
2020-04-19 ioncologyG ioncologyG
科学家们发现了一种通过破坏胰腺癌细胞的pH平衡来杀死癌细胞的新方法。近期,发表在Cancer Discovery上的这项研究报告了消耗离子转运蛋白的消耗是如何将pH值降低到损害胰腺癌细胞生长的程度的。
科学家们发现了一种通过破坏胰腺癌细胞的pH平衡来杀死癌细胞的新方法。近期,发表在Cancer Discovery上的这项研究报告了消耗离子转运蛋白的消耗是如何将pH值降低到损害胰腺癌细胞生长的程度的。
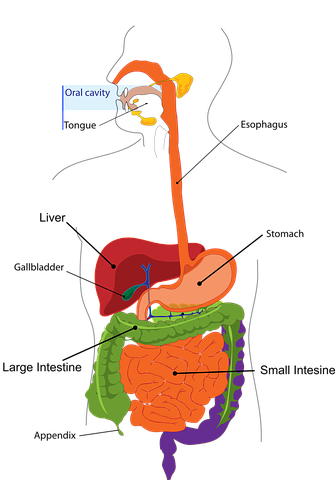
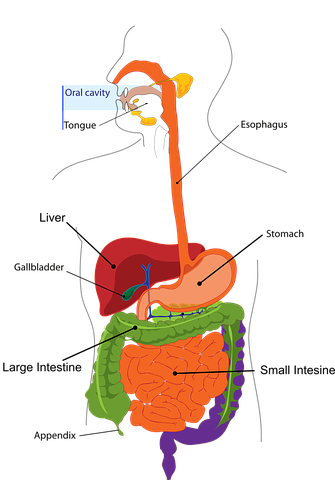
像所有癌细胞一样,胰腺癌细胞需要持续的能量来支持其生长和扩展。它们会增加正常细胞不使用的代谢途径,从而产生需要排出的多余酸。越来越多的科学家将注意力集中在控制癌细胞的pH值上,以此来治疗缺乏有效治疗方法的癌症。
桑福德伯纳姆普雷比(Sanford Burnham Prebys)国家癌症研究所指定的癌症中心助理教授Cosimo Commisso博士团队的研究表明,胰腺癌是目前尚无有效治疗方法的最致命的癌症之一,而干扰细胞的pH值代表了一种治疗胰腺癌的新方法,其中,一种名为“NHE7”的钠-氢交换器在胰腺癌中起着重要作用,通过抑制NHE7,我们可以促进癌细胞死亡。
氢-钠交换蛋白
钠-氢交换器的NHE家族是调节细胞及其细胞器(如核内体和高尔基体)内部pH值的转运蛋白,其位于细胞膜上,通过将氢离子(H+)与钠离子(Na+)交换而起作用,对细胞正常功能至关重要。
研究中,研究人员假设肿瘤细胞中产生的酸的增加可以作为治疗的易感点,并寻找专门针对这一点的策略。通过挖掘大量胰腺癌数据库,研究人员发现,与正常胰腺相比,胰腺癌中的NHE7水平更高,而预后最差的患者的肿瘤中NHE7水平最高。
在此基础上,研究小组开始了解NHE7在胰腺癌细胞中的作用。他们发现,NHE7定位于高尔基体并在此导入氢离子,形成酸性高尔基体和相应的碱性细胞质来支持癌细胞的新陈代谢。之后,研究人员开始进行实验是否可通过消除NHE7或使其失能来破坏碱性细胞质pH值,从而使胰腺癌细胞变得脆弱。
通过对胰腺癌细胞的一系列实验,研究小组发现,抑制NHE7会降低细胞质的pH值,从而引发细胞死亡。重要的是,在移植了人类肿瘤的小鼠中,去除NHE7会导致肿瘤缩小或完全停止生长。
Commisso博士指出,考虑到新确诊胰腺癌患者的5年生存率低于10%,显然目前急需更好的治疗方法,而找到新的癌症靶点有助于帮助我们制定治疗方案,并可能挽救更多患者的生命。这项研究表明,将pH平衡作为一种治疗胰腺癌的方法是有潜力的,下一步的研究将致力于找到抑制NHE7和抑制高尔基体形成酸性高尔基体的能力,如果成功,癌细胞将无法维持正常生长的pH值。
参考文献
Koen M.O. Galenkamp et al, Golgi Acidification by NHE7 Regulates Cytosolic pH Homeostasis in Pancreatic Cancer Cells, Cancer Discovery (2020). DOI: 10.1158/2159-8290.CD-19-1007
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#cover#
31
#Dis#
34
#阻断#
37
#ISC#
28